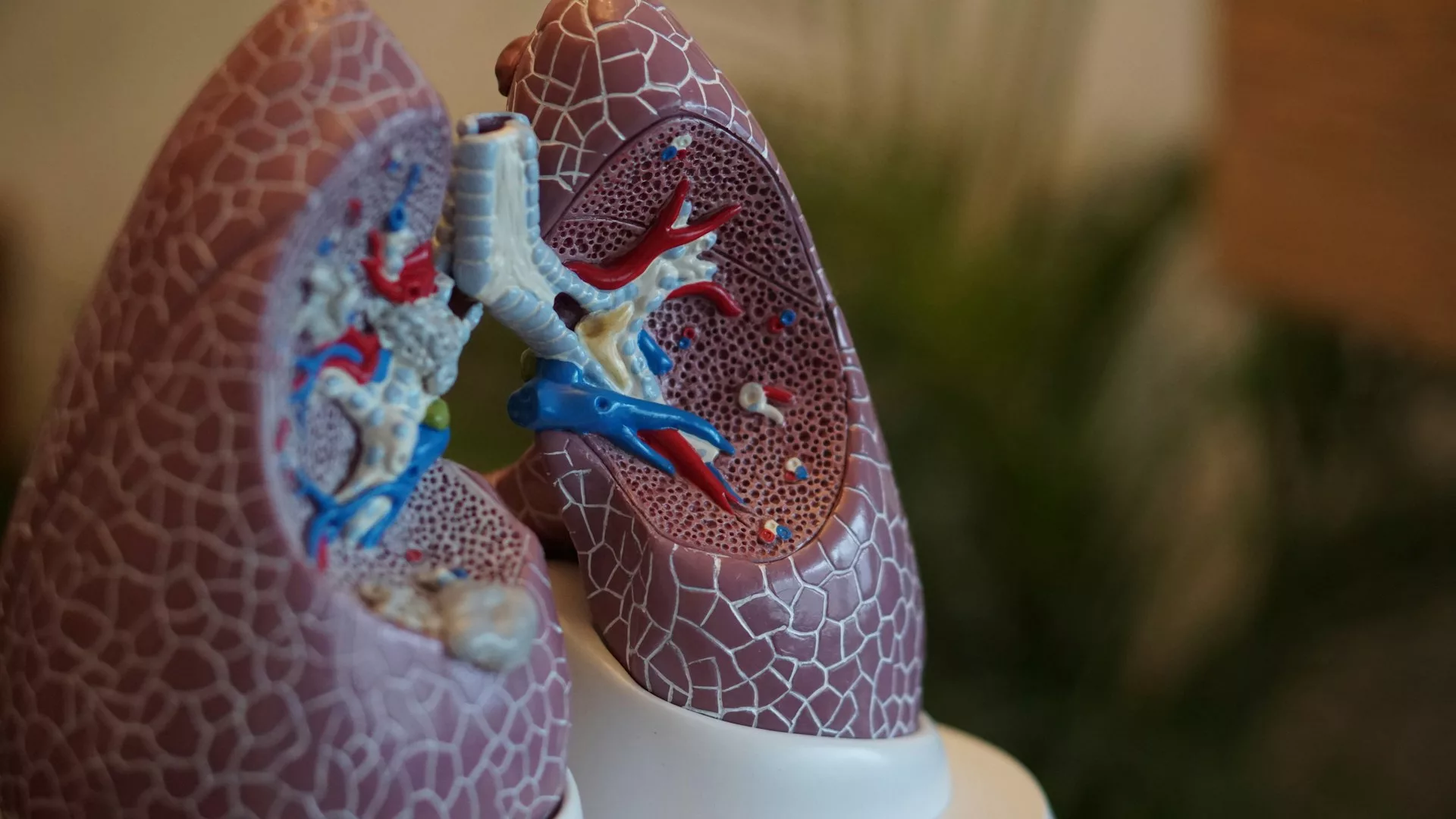
We have co-evolved with numerous microorganisms, the ‘microbiota’. The role of these organisms in the respiratory tract is only just being appreciated. Photo credit: Robina Weermeijer via Unsplash
Despite a reciprocal relationship prevailing for millennia between us and our microbiome, we have only recently started to appreciate the extent to which we coexist with our microscopic cohabitants. In 2007, the Human Microbiome Project aimed to catalogue the diversity of microbes which take advantage of the hospitable environments we provide.
For a long time, scientists maintained that, when healthy, the LRT [lower respiratory tract] would be void of a microbial presence.
Though it contributed to the understanding of our own microecology, the project fell victim to a common omission—it ignored the lower respiratory tract (LRT), which consists of the trachea, bronchial tubes, and lungs. Like most research before it, the project focused on the upper respiratory tract (URT), composed of the nose, mouth, sinuses, pharynx, and larynx. For a long time, scientists maintained that, when healthy, the LRT would be void of a microbial presence. An interest in this region has only commenced in the last 10 years.
Why is the lung microbiome significant?
Unlike the gut, microbial flow along the respiratory tract is bi-directional and unfiltered, making it much more dynamic than the gut in terms of community make-up. Observations of the URT suggest it has a different community composition to the LRT within and across individuals. One example is the presence of Proteobacteria, such as Pseudomonas and Haemophilus, which are more common in the lungs.
The possibilities open to us through engineering these communities are endless. We could inoculate hospital ventilation with commensal (non-harmful) organisms, reduce niches (roles within the environment) available to pathogens, or predict disease progression and prevalence based on lung community structure. Understanding the composition and dynamics of microbial communities could be key to realising these possibilities. The dynamic nature of the respiratory tract primes it for these purposes, enabling desirable microbes to enter and settle.
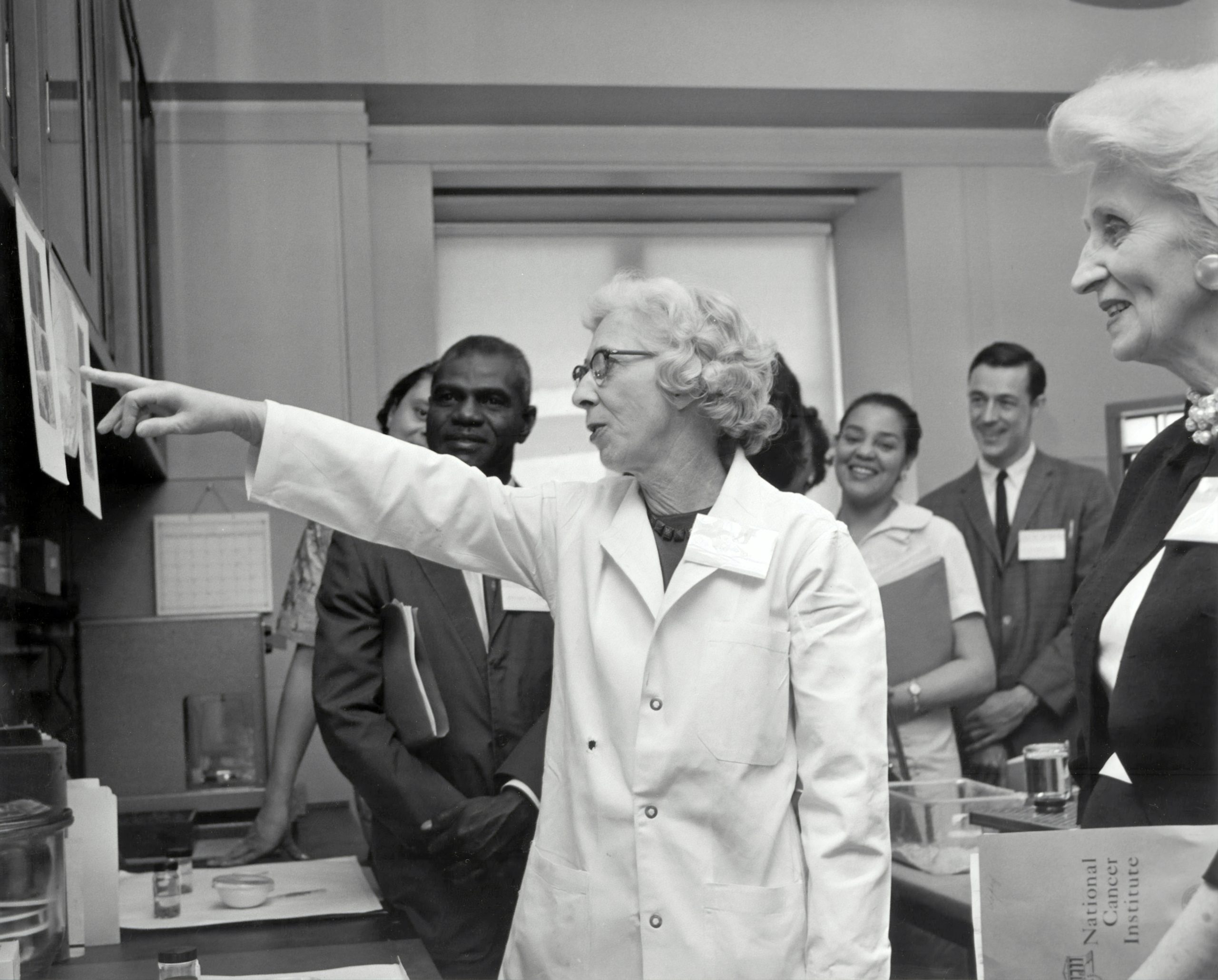
Until recently, the lungs’ microbiome has been largely under-researched.
So, who are these unexpected guests?
There are a few groups of bacteria known to colonise healthy lungs. For example, Streptococcus spp. are common within the respiratory tract. Despite their notoriety as the pathogen underlying strep throat, they play an important role in the microbial community as a commensal organism. Alongside Prevotella and Pseudomonas spp., they help take up niche space otherwise used by pathogens and regulate the immune response to the microbiome. Mice grown in sterile conditions without Streptococcus spp. develop stunted immune systems, showing disproportionate reactions when later exposed to microbes. Recent studies have even proposed that the bacteria could play a vital role in delivering viral antigens to the host’s immune cells. Similarly, Candida spp. are fungi found commonly on mucous membranes which have gained mistrust due to their role in thrush infections. The fungi are just as common in diseased lungs as they are in healthy lungs, becoming pathogenic by currently undetermined external factors.
When pathogens invade—upsetting the balance between the resident commensals—the stability of the microbiome can break down (known as “dysbiosis”). In these cases, disease can progress more quickly, taking advantage of the community to bolster their attack.
How can we avoid dysbiosis?
Administration of positive bacteria has been shown to combat a variety of diseases, including cancer. For example, administering doses of therapeutic probiotics containing Lactobacillus spp. has already been shown to reduce the side effects of treatments like chemotherapy. Furthermore, inhalation delivery of E. coli containing a cancer treatment drug improved cancer cell death rate.
Next steps in this treatment may include engineering the bacteria to produce the therapies themselves rather than acting as a vessel. Alternatively, research could examine potential for altering the longevity of said bacteria in the lungs. These engineered bacteria could become integrated into an individual’s microbiome, allowing for improved response and lowered risk of cancer development and progression.
Until recently, the lungs’ microbiome has been largely under-researched. With the accumulation of exciting novel findings and the advent of new technologies, microbial communities open exciting possibilities for research. Let’s work with our unexpectedly important guests and elevate them to a trusted position in our microbiome.