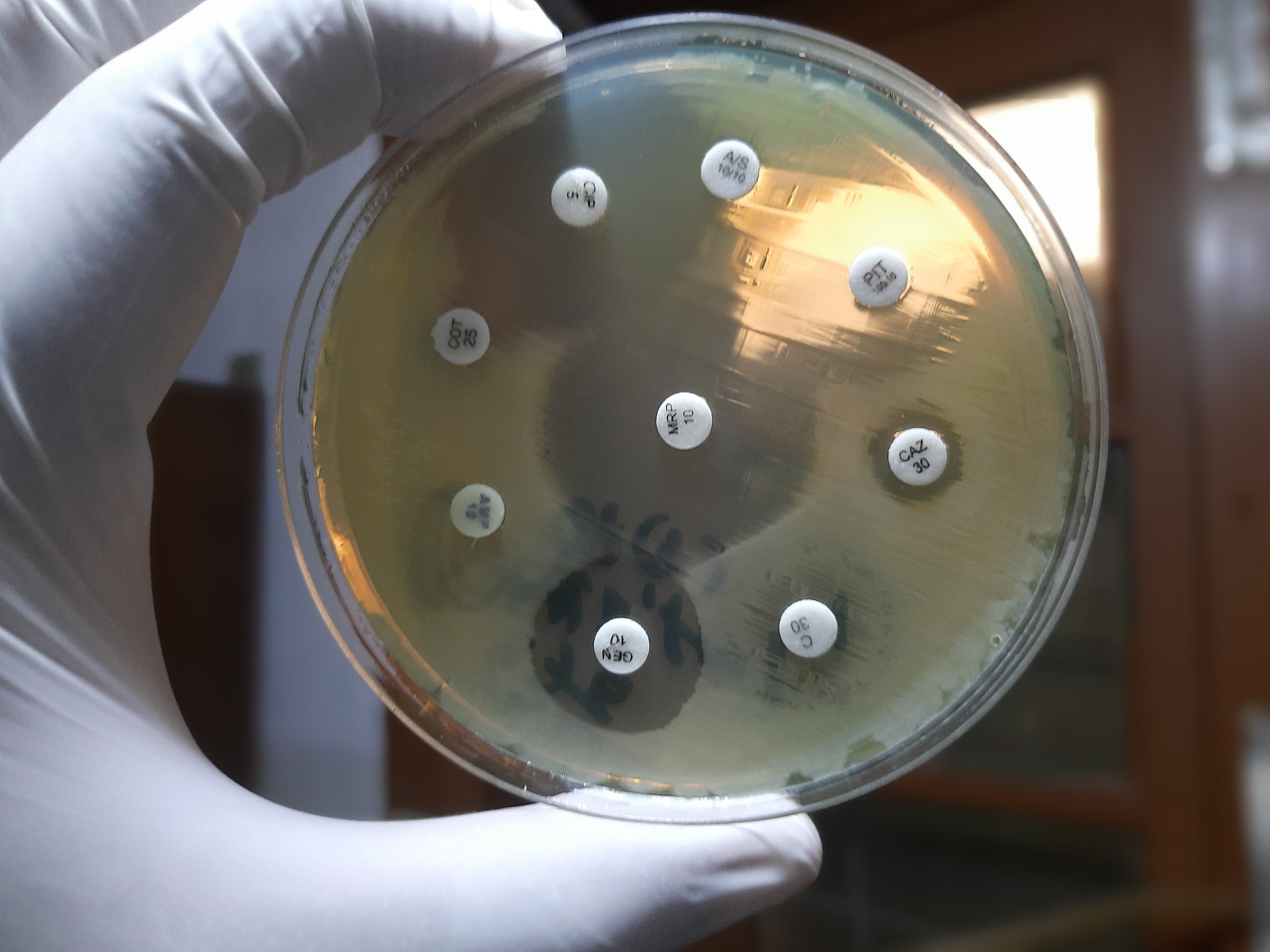
Ajay Kumar Chaurasiya, CC BY-SA 4.0, via Wikimedia Commons
A study by the University of Oxford has reported evidence for the translocation of antibiotic-resistant bacteria from the gut to the lungs. In today’s landscape of increasing antimicrobial resistance (AMR), this new pathway via which resistance can develop and spread in a single patient poses a risk to the efficacy of modern medicine against infections.
The study led by the Department of Biology of the University of Oxford monitored a single patient as part of the ASPIRE-ICU epidemiological study. A course of the antibiotic meropenem was initially given to the patient to treat a urinary tract infection.
While this treatment killed off the infection-causing bacteria and other non-resistant bacteria, meropenem-resistant Pseudomonas aeruginosa proliferated within the gut and was later found in the lungs.
Colonies of the same species of bacteria being found in both the gut and the lungs is not unheard of, but the dynamics of this translocation are poorly understood. By tracking how samples of P. aeruginosa colonies from the patient evolved over time, the authors could draw a relationship between the colonies found in the lungs and those within the gut.
This phylogenetic method provided definitive evidence that ‘lung colonisation in the ICU was driven by the translocation of P. aeruginosa from the gut’.
There are thought to be three primary mechanisms inhibiting bacterial translocation in a healthy individual.
The first is the integrity of the epithelial layer of the gut, one of its four layers of specialised tissues. The epithelial layer is crucial for digestion of food and absorption of nutrients, but also tightly regulates what can and cannot leave the gut and enter via the bloodstream. This means that while the gut lumen is populated by a large and diverse microbiome composed of hundreds of bacterial species, the exterior layer of the intestines is essentially sterile.
Supporting this physical barrier against gut permeability is the equilibrium within the gut environment—indigenous microflora prevents bacterial overgrowth.
A healthy immune system serves as the last line of defence: any translocating bacteria should be quickly detected and neutralised.
This spells bad news for many critically ill patients in hospitals, where all three mechanisms may be compromised. Chronic and critical illnesses notably induce intestinal permeability and promote death of the cells lining the epithelial layer.
Furthermore, the microbiome undergoes dramatic changes during illness, with a reduction in anti-inflammatory bacteria and a proliferation of disease-promoting bacteria. This is only worsened by the use of antibiotics to treat infections, which are common among patients in the ICU.
Like the patient in the Oxford study, antibiotics are a cornerstone treatment against infection, but allow for proliferation of resistant bacteria, worsening the imbalance of the gut microbiome.
Finally, hospitalised individuals are more likely to have compromised immune systems as a result of conditions like autoimmune diseases, cancer, and sepsis, weakening their response against bacterial translocation from the gut.
The patient in the study fortunately exhibited an immune response against the lung infection, avoiding development of the infection into pneumonia.
Others may not be as lucky. P. aeruginosa poses a significant risk of serious or fatal infections among those suffering from cystic fibrosis, undergoing surgery, or placed on medical equipment like catheters and ventilators.
P. aeruginosa infections are particularly difficult to treat due to the intrinsic antimicrobial resistance of the bacterium, having mechanisms in place to pump antibiotics out of the cell and inactivate antibiotics, and its ability to evolve AMR to escape the action of the most readily available antibiotics.
In a 2017 report by the World Health Organisation, P. aeruginosa was classified among the “critical” group of bacteria for which the development of new antibiotics is of the highest priority.
Another finding of the study is the accelerated rate of evolution of P. aeruginosa in critically ill patients, increasing the rate of development of AMR.
Further, bacterial translocation is associated with greater risk of developing critical illness: a study at the Scarborough Hospital revealed that gut bacteria were responsible for 74% of postoperative complications in patients undergoing laparotomy, and patients with evidence of gut translocation were three times as likely to develop sepsis.
In policies against AMR, there is thus a need to consider the development and spread of resistance within an individual, and to develop effective solutions against bacterial translocation.
The lead author of the Oxford study, Professor Craig MacLean, suggests exactly that. He proposes that there are benefits to ‘eliminating AMR bacteria from the gut microbiome of hospitalized patients, even when they are not actually causing infection’.
This approach of prophylactic antibiotic therapy—antibiotic treatment to prevent rather than treat infection—must be used conservatively to avoid toxicity associated with overuse of antibiotics, and of course to prevent development of AMR.
Antibiotic prophylaxis against P. aeruginosa is particularly risky—few antibiotics exhibit activity against multidrug-resistant P. aeruginosa. The overuse of these antibiotics as a pre-emptive measure against bacterial translocation will only provide the impetus for P. aeruginosa to develop resistance more quickly against new drugs.
There is a need to understand how frequently gut to lung bacterial translocation occurs, and the severity of such translocations developing into serious infections. This will allow us to understand the risks of bacterial translocation and weigh the benefits of using antibiotic prophylaxis. Until then, antibiotic prophylaxis remains an unrealistic solution.
Nonetheless, the Oxford study has demonstrated the implications of gut-lung translocation and the urgent need to develop therapies against it, and AMR as a whole.