Over the last few decades, our treatment of cancer has been revolutionised. The field has been transformed by a focus on ‘personalised medicine’ which involves treating patients’ individual cases rather than grouping them together. It is universally recognised that there is no single cure for cancer, and increasing evidence suggests that there is not a ‘one size fits all’ treatment, even within the same cancer types.
One cutting edge advance revolutionising the field involves the use of a patient’s own immune cells to fight their disease. Cancer is often described as a ‘war’ and this process effectively provides the body with the necessary weapons to battle the cancer.
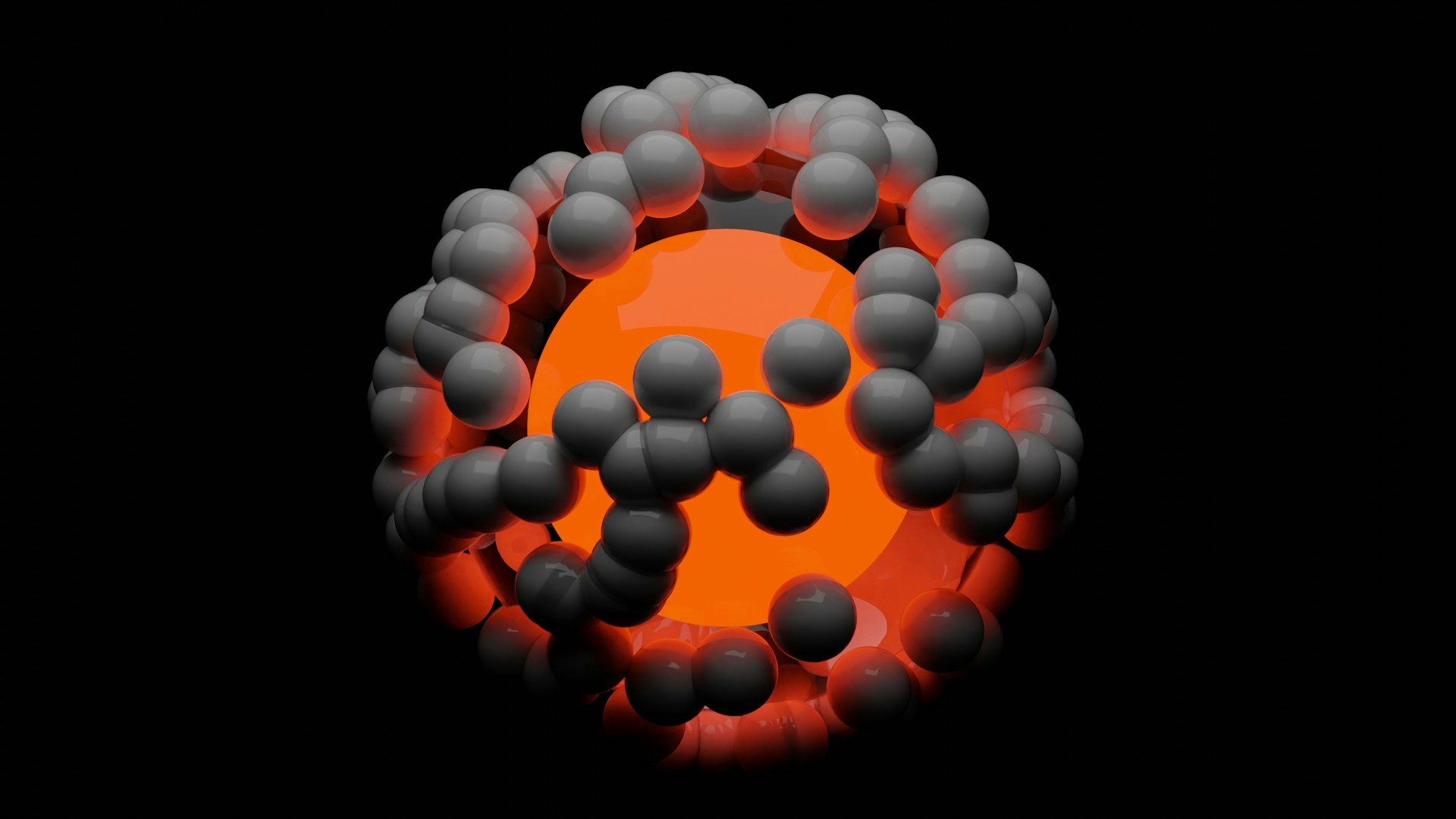
The cells used are known as chimeric antigen receptor (CAR) T cells and are modified versions of immune cells which normally recognise and kill pathogens such as bacteria and viruses, but they can also target cancerous cells. They achieve this through recognition of short protein sequences on the cell surface known as ‘antigens’ which signal that the cell is abnormal. Once this signal is received, the T cell is then able to kill the cancerous cells and spare the surrounding healthy tissue.
This technology is a far cry from chemotherapies used in the 1940s to treat cancer. These drugs, known as ‘nitrogen mustards’, were initially used in chemical warfare but were identified to specifically target dividing cells. At the time, little was known about cancer cells other than their unusually rapid division, so this was the only way the cells could be targeted. Unfortunately, cancerous cells are not the only bodily cells to divide so cells such as hair follicles and immune cells were also killed. This led to the catastrophic side effects often documented during chemotherapy including infertility, hair loss and immune suppression.
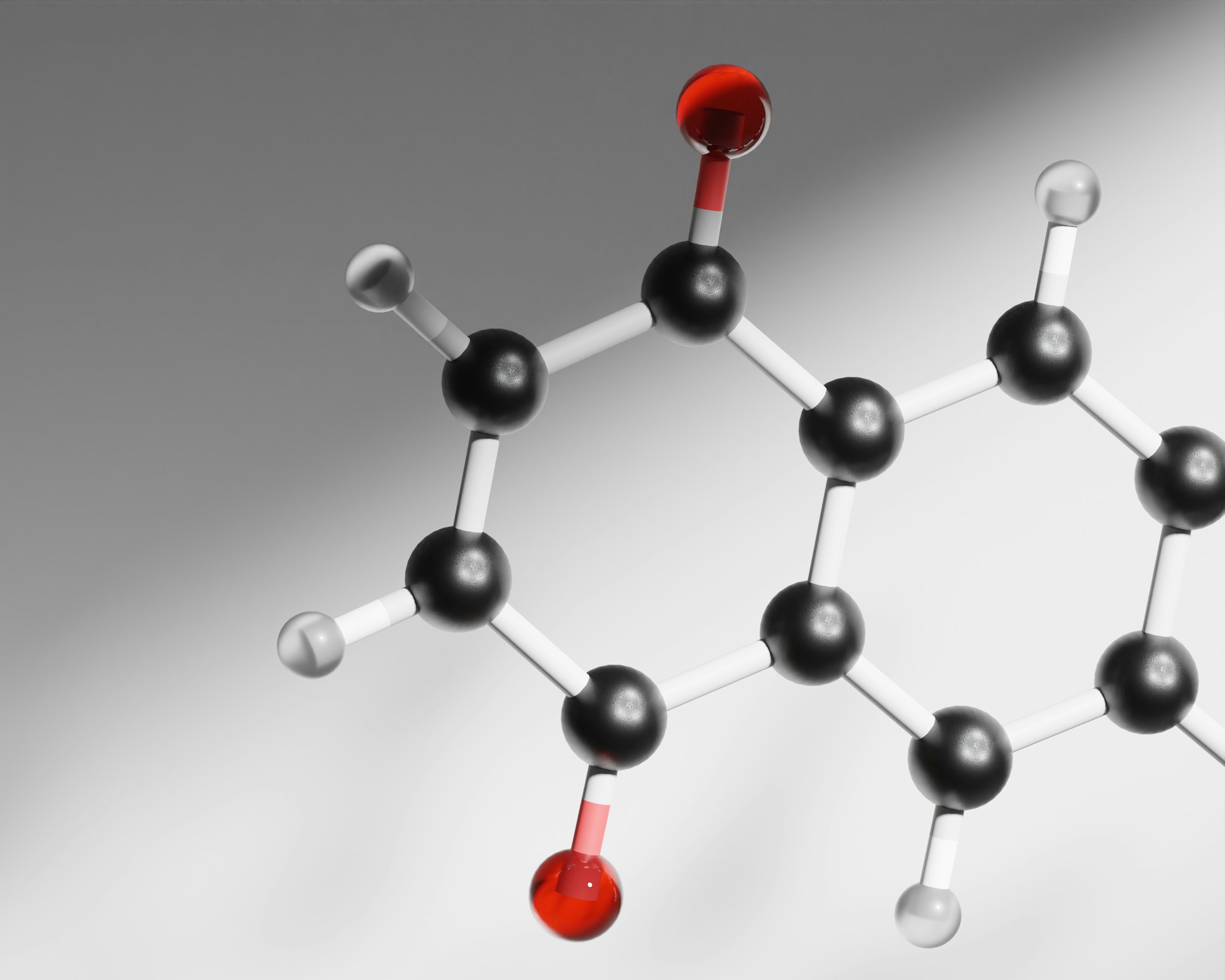
In modern treatment, some cancers can be identified by highly specific ‘biomarkers’ which are molecules that exist solely on the cancerous cells. These allows drugs to be developed specifically to target individual cancer variants, meaning more effective treatments and fewer harmful side effects. Partly due to development of these sorts of drugs, breast cancer now has around a 90% cure rate if diagnosed early and prognosis is generally improving at an astonishing rate.
It is difficult to pinpoint exactly when the treatment of cancer turned the corner from the use of drugs which are effectively poisons to innovative and precise technologies such as CAR T cells. One turning point was provided by Hanahan and Weinberg who published the seminal paper: ‘the Hallmarks of Cancer’ in the year 2000. This defined a new set of traits common to all cancer cells, allowing new targets to be developed. Their original study has been developed since, but can be seen as a basis for most modern forms of treatment.
A key concept set out in this paper that led to the use of immunotherapies is the concept of a ‘tumour microenvironment’. For cancer cells to maintain their high rate of division they must modify local tissue through the dysregulation of normal signalling pathways. Through this process, cells can promote the growth of new blood vessels, inhibit programmed cell death (which would normally be stimulated in response to detection of DNA damage) and, crucially, suppress the immune response.
Immune suppression by cancer generally prevents recognition of the tumour by immune cells such as the T cells mentioned earlier. The precise mechanisms by which the cancer hides vary, and research is ongoing in this area. Oxford professor Vincenzo Cerundolo at the MRC Weatherall Institute of Molecular Medicine recently showed that secretion of an enzyme by tumour cells was implicated in immune suppression during acute myeloid leukaemia (AML).
Leukaemias have traditionally been some of the hardest forms of cancer to treat, due to the lack of a solid tumour mass rendering operation impossible. The disease is the second most common form of cancer in adults and the most common in children. Research by the National Cancer Institute showed that through CAR T cell therapy, 90% of patients were cured of the condition with no relapse, compared to the normal 27% survival rate for the disease Staggering results such as these provide hope for the future of cancer therapy, with more targets being developed to treat different forms of cancer. Although personalised treatments are expensive, companies such as Oxford-based Adaptimmune are already being licensed to produce the T cells, so their use in the general population is by no means impossible. These forms of novel therapy will hopefully ensure that the war against cancer is one we do not lose.