Income inequality and food insecurity contribute to poor microbiome health in underprivileged socioeconomic groups. Photo credit: julien Tromeur via Unsplash
Those with a keen eye or even a partial awareness of gastronomy may have noticed an uptick recently in the number of products and influencers emphasising the importance of the gut for our wellbeing and health. This boom has coincided with an increasing number of supermarket goods brandishing themselves with catchy taglines such as “live culture” or “fermented” that promise to deliver a multitude of benefits impacting digestive, immune and cardiovascular health. It feels like everywhere one looks is a jumble of kombucha, kefir, and kimchi.
While the gut has been brought to the forefront of contemporary health discourse, with a particular focus on fermented food and bacteria, the more inquisitive among us might wonder exactly why our digestive system is so incredibly important beyond simply doing the job it says on the tin.
What is the gut microbiome?
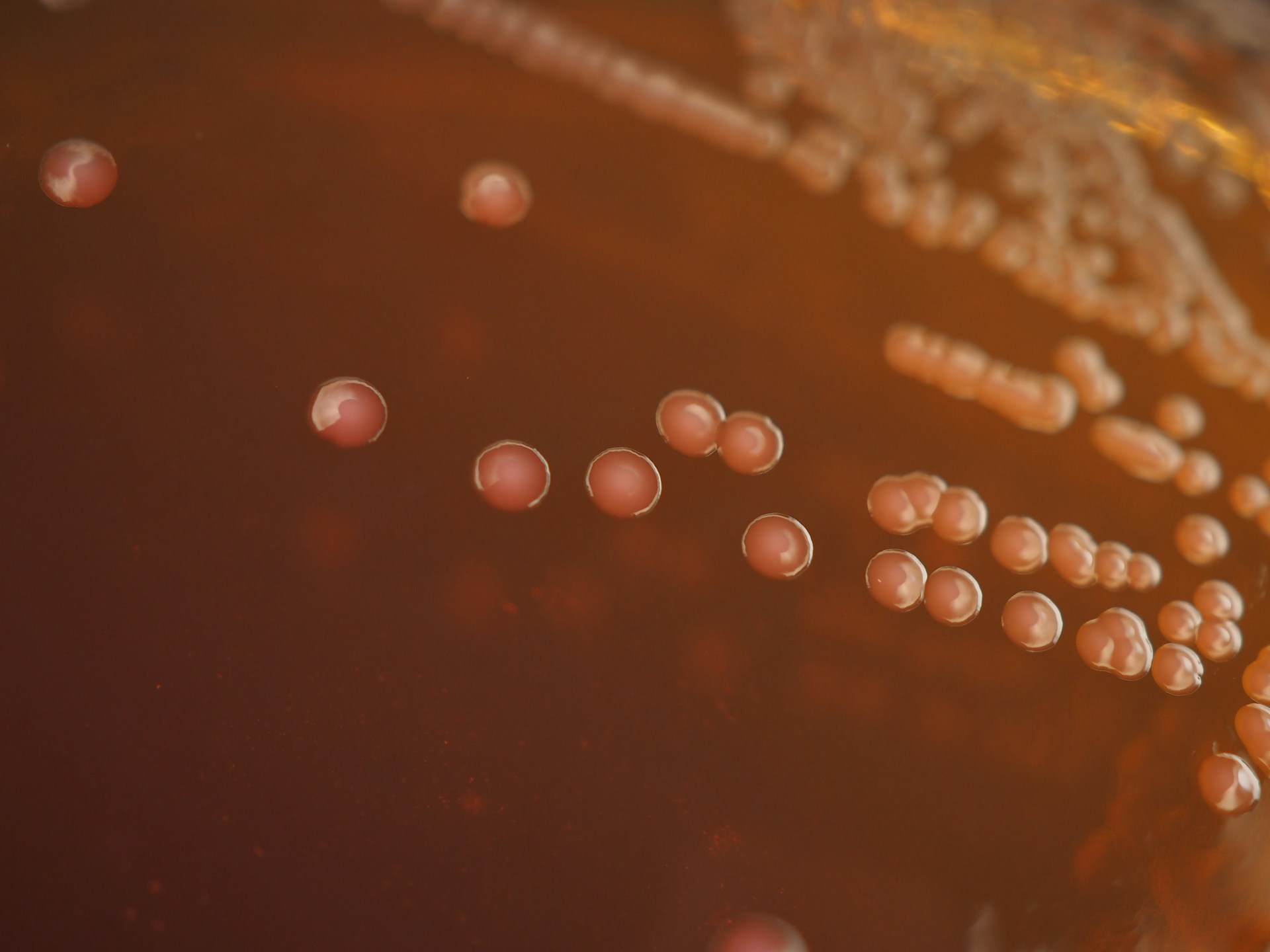
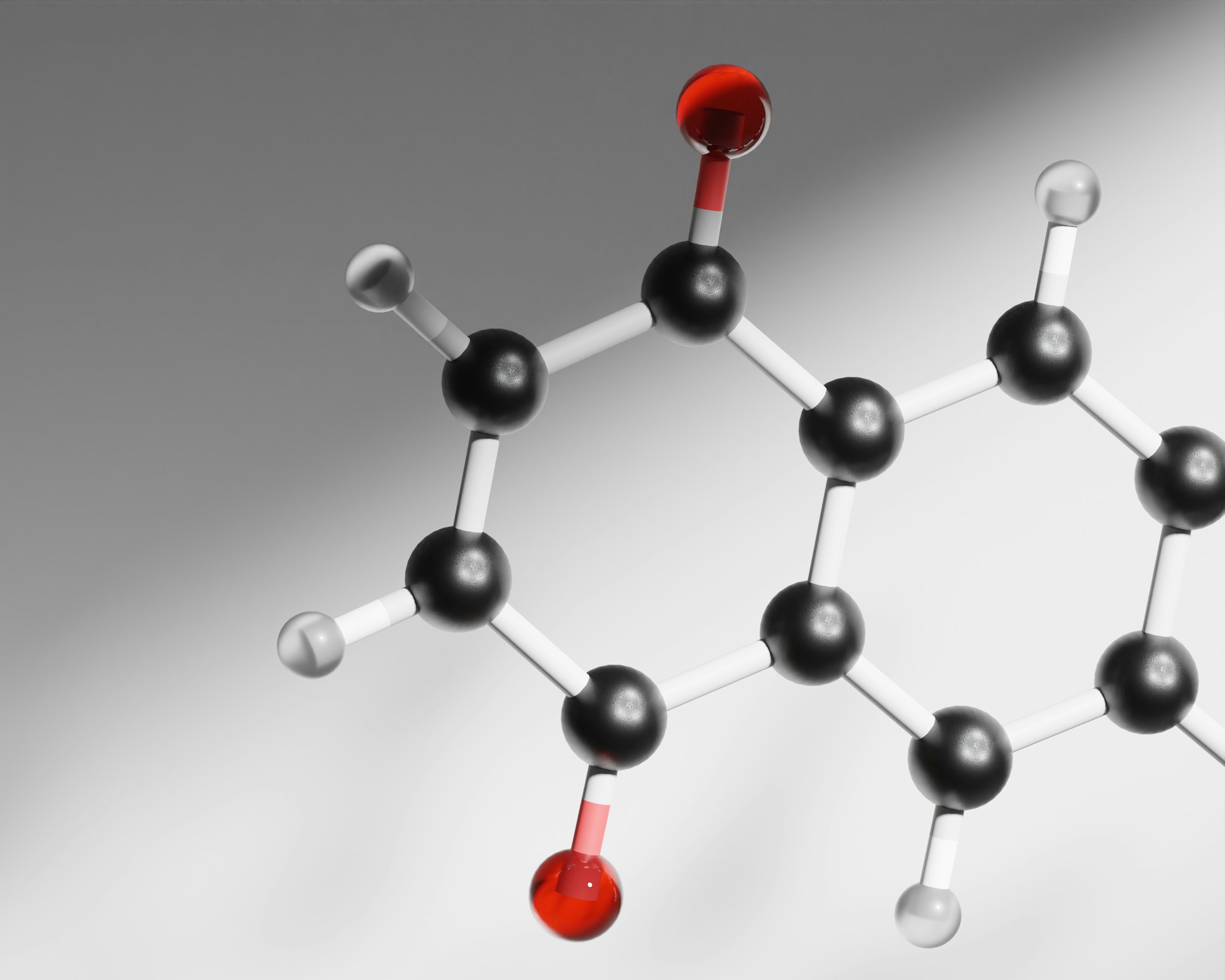
Though lots of this seemingly boils down typical faddish consumerism espoused by companies seeking to make profit (e.g. coffee enemas that supposedly ‘improve gut health’, a claim currently rejected by science), much of the logic is rooted in the gut’s curious ability to form associations with trillions of beneficial microbes that help sustain its health and metabolism. This is the microbiome, encompassing the total volume of microbial occupants in the human gastrointestinal tract, including many different bacteria, viruses, fungi and more.
Without them [gut microbes], the human body would struggle to execute tasks like combating infection…
Such symbioses between the gut and its microbes allow the microbiota to obtain goods like protection and nutrients in exchange for supporting processes in our bodies involved in immune modulation, nutrient extraction, and hormonal regulation. Without them, the human body would struggle to execute tasks like combating infection or obtaining the many nutrients it relies on the microbiome to extract from food.
That is why maintaining sustainable gut microbiome ecology—by nourishing and supporting the microorganisms that keep our bodies healthy and strictly avoiding behaviours like drinking or smoking that can damage the microbiome—becomes important.
How socioeconomic status affects the gut microbiome
While this seems straightforward, dysbiosis (damage to our microbiome) is not always caused by such deliberate actions. Many factors such as genetics, food insecurity, and even pollution having a contributing role. As one study has found, the level of one’s socio-economic status also plays an equally important role, with several of its findings pointing to multiple noticeable influences on the microbiome associated with its variation.
The study, led by Ibrahim Zuniga-Chaves at the University of Wisconsin-Madison, is one of the first of its kind to offer an in-depth perspective into the role of neighbourhood-level socioeconomic status (SES) in modulating the human gut microbiome. To do so, the team investigated the interplay between different social factors, such as diet, health, income, and race, and their manifestation in affecting microbiome composition, and assessed the prevalence of four bacterial groups displaying antibiotic resistance (i.e. multidrug resistant organisms, MDROs) across the different groups. This was followed by assessing the level of serious infection caused by these MDROs across various sites of the body like presence of skin lesions, blood and urinary tract infections, and diarrhoea, dehydration or weight loss.
MDROs usually arise from improper antibiotic use, and in many cases are easily spread through direct contact from individual to individual. The effect these microbes have on the microbiome is largely, and unsurprisingly, negative. By further reducing gut microbiome diversity, and increasing the likelihood of severe infection and disease, their presence poses an even greater risk for already vulnerable groups susceptible to these types of conditions.
…greater hardship neighbourhoods… were found to have a less diverse range of species occupying their microbiomes than those from the wealthier cohort.
Individuals belonging to lower SES and higher economic hardship index groups (EHI) were found to more likely have a lifestyle with factors detrimental to microbiome health, such as having greater food insecurity, reduced access to nutrient-rich foods, greater consumption of high-fat and low-fibre foods, and restricted access to healthcare. These factors were reflected in the microbiome composition of the different socioeconomic groups: greater hardship neighbourhoods (those with greater poverty status, crowded housing, lower education) were found to have a less diverse range of species occupying their microbiomes than those from the wealthier cohort.
This is of concern to many. Reduced diversity in the microbiome has been linked to increased prevalence of various diseases including irritable bowel syndrome (IBS), obesity, neurological disorders, and cancer. Fewer commensals (neutral bacteria that benefit from a human host without causing any adverse or beneficial effects) in the gut also opens up space for pathogenic species to colonise and take over and allow diseases such as multiple sclerosis to emerge. More diversity also allows the microbiome to assist a wider assortment of host functions like intestinal homeostasis, food digestion, and even neurological conditions or mental health.
On the species level, low SES individuals possessed more Holdemanella, Catenibacterium, Megasphaera, and Atopobium,bacteria associated with obesity-associated insulin resistance, dyslipidemia, and Crohn’s Disease. Conversely, wealthier cohorts had greater amounts of Akkermansia, which reduce the risk of obesity, Type two diabetes, IBS, and cancer. The study also tested higher for levels of Lachnospiraceae and Ruminococcaceae that aid in the body’s digestion of fibre and enhance gut immune function.
These differences were hypothesised to be brought about by the dietary habits between the two groups, with low SES families in the USA being subject to ‘high added-sugar, [and] low fibre diets’. After compiling and comparing the effects of various social factors driving this disparity, food insecurity was found to play the biggest role in these compositional differences, further emphasising the importance of nutritional food for gut microbiome health.
The group then moved to analysing MDRO prevalence across the different groups and found these antibiotic-resistant species to have a greater distribution in low SES and high EHI microbiomes. This was likely owing to greater levels of poor nutrition, chronic stress, and inflammation observed in these communities.
Sociological implications
Despite only looking at US neighbourhoods, the findings of the study likely pose important implications for us all, with global income inequality remaining sky-high over the past century (affecting 71% of the population), and the cost of living crisis hitting more families in the UK than ever before.
Food poverty plays a very critical role worldwide, with globally 783 million people currently experiencing chronic hunger, three billion people unable to afford a nutritious diet, and 45% of deaths among children under five being linked to malnutrition. One of the biggest drivers of global food poverty can be attributed to the income inequality that exists between the society’s wealthiest, with the top 1.1% of the global population holding 45.8% of the globe’s total wealth, and those 670 million people living under extreme poverty.
This, combined with reduced access to healthcare (affecting three and a half billion people globally), puts those living below the global poverty line at extra risk of health complications, both microbiome dysbiosis-associated and as a whole. Not only that, but as more people struggle to make ends meet (including those in food-secure nations) these figures will only climb higher and get worse.
Overcoming these challenges will be a difficult feat to accomplish, with progress slow and taking several years at the very least. Regardless, we must start to come up with tangible solutions to tackle the issues of food insecurity and poor microbiome health. Some good starting points involve looking at the root causes of these problems, such as reducing global income inequality, eradicating food insecurity and famine, and developing solutions for socially accessible healthcare. These can all contribute to reversing the effects of global income and food poverty and hopefully improve not only microbiome health, but our general health too. Whether these objectives will go on to be accomplished under the status quo offered by the current system, only time will tell. Yet one thing is obvious—the gut feeling likely plays a bigger role than most of us think.