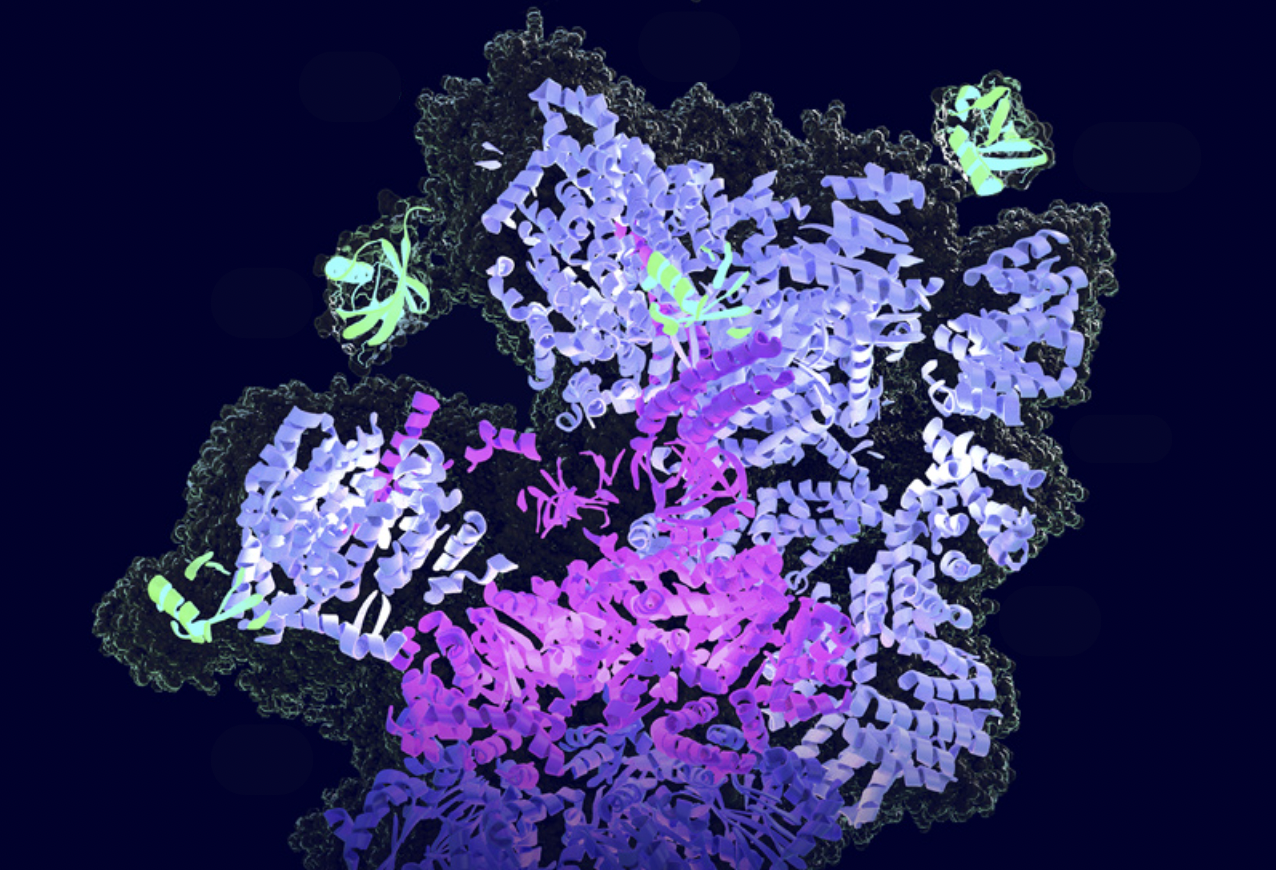
Exploring how PROTACs are revolutionising the approach to treatment. Image credit: SFB F79 Targeted Protein Degradation, from a press release.
In a healthy cell, the process of protein degradation or breakdown, called proteolysis, into peptides and ultimately amino acids is a very normal phenomenon. This process, which is carried out by a complex of proteins called the proteasome, targets proteins that have been misfolded so their function as an enzyme is no longer effective. It was with a view to breaking down disease-causing abnormal proteins that PROTACs (proteolysis targeting chimeras) were chemically produced.
PROTACs are emerging as a promising new therapy in the face of the limitations of small molecule inhibitors (SMIs). SMIs are used to inhibit proteins involved in diseases. Since their advent in the early 2000s, SMIs have revolutionised a number of treatments, particularly cancer therapy, with 88 SMIs approved by the United States FDA since 2001. However, we face challenges in terms of their efficacy, selectivity and drug resistance.
One of the disadvantages of SMIs is that they can’t bind to proteins that don’t have an active site to which they can bind. These proteins are grouped together under the name “undruggable”. SMIs are needed to be given in a high concentration over a period for the treatment to be effective, which can lead to side effects of inhibition or activation of other proteins. They also don’t bind to the active site of proteins whose 3D structure has changed considerably due to excessive mutations in genes, particularly in cancer cells. This leads to the drug resistance phenomenon which can be tackled using PROTACs.
Unlike SMIs that inhibit proteins, PROTACs work by degrading them. This is done through a catalytic process, allowing PROTACs, unlike SMIs, to be reused. They can therefore be administered at lower doses. Since PROTACs don’t target enzyme active sites and mainly target well-conserved protein motifs, that is, protein sequences that are not subject to mutations, they can tackle previously “undruggable” proteins and prevent drug resistance.
The future of PROTACs lies in their optimisation.
Since the synthesis of the first PROTAC in 2001 by Sakamoto’s team, they have continued to be improved with the aim of ultimately being used clinically. In 2020 and 2021, two PROTACs developed by the US biotech company Arvinas were entering phase 2 clinical trials to treat prostate cancer and breast cancer. Currently, since December 2022, one of the PROTACs developed by the company (ARV-471) has been undergoing phase 3 clinical trials to determine its safety and therapeutic efficacy compared with current FDA-approved treatments for advanced metastatic breast cancer. The results of this trial could reveal a lot about how PROTACs can be used as a cancer treatment option in the future.
The future of PROTACs lies in their optimisation. The development of PROTACs that could be activated through a light signal, could result in a time- and space-dependent breakdown of proteins or the development and synthesis of new binding proteins could be used to be more tissue-specific, cell-specific or even cancer-specific. The results of the ongoing PROTAC clinical trials are key to advancing the drug discovery process and contributing to the treatment or fight against a number of diseases.