NIH Image Gallery from Bethesda, Maryland, USA, Public domain, via Wikimedia Commons
In the years preceding 1964, Dr John C Steele, J C Richardson and Jerzy Olszewski faced a conundrum: patients experiencing a series of motor issues that had never been characterised before. With symptoms including an unsteady gait, a downward gaze, and problems swallowing, the patients puzzled this group of clinicians.
In their 1963 report, the cluster of symptoms was first officially described. The report contained an anecdote of a wife who found her husband ‘a little slower in thinking’ than usual. His main symptom developed over time, as he struggled to gaze downwards at his watch. In 1964, Steele, Richardson, and Olszewski published a paper that shifted the paradigm. Here, for the first time, they named this disease as progressive supranuclear palsy, or PSP.
Under the microscope
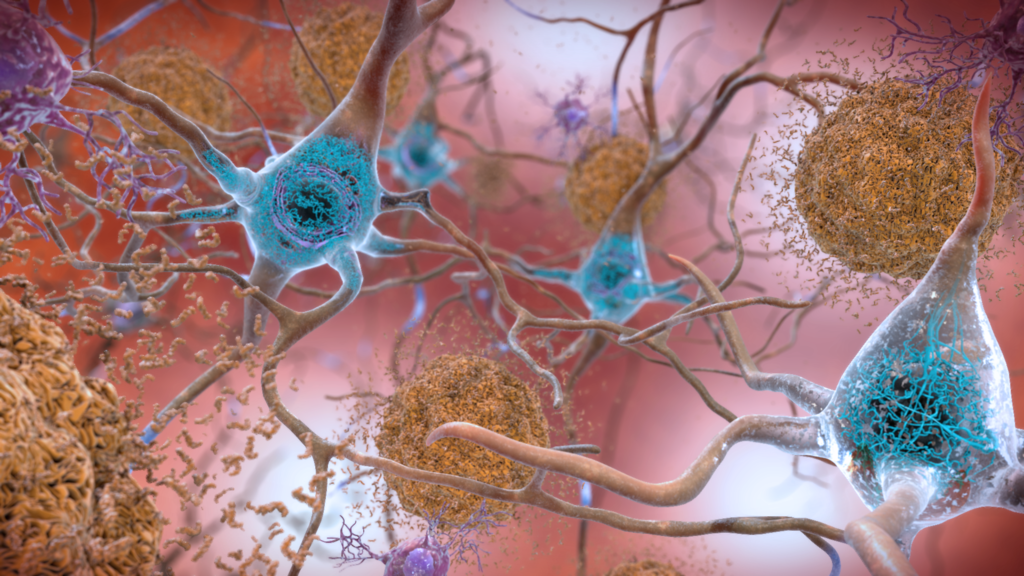
Since its initial identification, PSP has become better understood and is now classified as a tauopathy. In other words, PSP falls under a category of neurodegenerative diseases, which also includes Parkinson’s and Alzheimer’s disease, characterised by the deposition of abnormal versions of a protein known as “tau” in the brain. In its healthy form, tau has vital functions in maintaining microtubule dynamics. Microtubules act like a cellular skeleton, ensuring the insides of cells are organised, and that molecules can be moved effectively within cells.
Tau can exist in various forms called isoforms, specifically 3-repeat (3R) and 4-repeat (4R) taus. These isoforms result from different alternative splicing patterns of RNA, which act as a template for synthesising the tau protein. The tau-encoding pre-mRNA contains both exons (protein-coding RNA) and introns (non-coding RNA). Alternative splicing removes different combinations of these introns and exons from the tau-encoding RNA, allowing one gene to give rise to multiple tau isoforms.
When exon 10 is spliced out of the RNA, 3R-tau is formed. If exon 10 remains included in the RNA, then 4R-tau is formed. Healthy adults should express equal amounts of the two isoforms. This balance between 3R- and 4R-tau is tightly controlled by the regulation of alternative splicing.
In PSP, abnormality in the regulation of alternative splicing means that exon 10 is included in the RNA more frequently than it should be. This overproduction of 4R-tau disrupts the balance of 3R- and 4R-tau in the brain. Accumulated 4R-taus aggregate to form a mix of twisted and straight filaments called neurofibrillary tangles (NFTs), which damage neuronal cells in the brainstem, cerebral cortex, cerebellum, and basal ganglia. These regions of the brain are responsible for controlling motor function, eye movement, and sensory processing among other functions. As a result, the accumulation of 4R-tau leads not just to neurodegeneration but also to the debilitating symptoms of PSP.
A process of elimination
PSP is incredibly difficult to diagnose. As a neurodegenerative disease that is rarer than diseases such as Parkinson’s and Huntington’s disease, but shares symptoms with them, misdiagnosis is rife. In addition, despite the albeit limited understanding of the disease we do have, there is no single diagnostic test that identifies PSP. Instead, a diagnosis can only be made by physiological and neurological evaluation for traits that subtly differentiate an individual’s symptoms from those observed in other neurodegenerative diseases.
For example, a clinician may initially assess for “axial rigidity”, where individuals fall or tilt their heads backwards as opposed to forwards, as more commonly observed in Parkinson’s disease. A neurological evaluation using MRI or PET scans can also identify shrinkage at the top of the brain stem, characteristic of PSP. Patients are then given treatments for other neurodegenerative diseases, and the effects are monitored.
For example, one drug often prescribed is levodopa, which is used to treat Parkinson’s disease. In the brain, levodopa is processed to form dopamine, which is severely lacking in individuals with Parkinson’s disease. If the drug works in alleviating their symptoms, the patient likely has Parkinson’s disease. If not, they may have PSP, but there is no way to confirm this.
Due to this uncertain diagnostic method, statistics surrounding PSP vary greatly. In fact, Professor Huw Morris at the PSP-PROSPECT study recently revealed that ‘the disease may be twice as common as previously thought’. Yet, one thing is certain: PSP is still considered very rare with only around 4,000 people currently diagnosed with the disease in the UK. This rarity leaves many diagnosed feeling ‘challenged by the lack of PSP research, lack of funding for such research, and/or failure of health care providers or PSP organisations to communicate findings’. It is vital that those diagnosed with PSP feel included in the conversations and discoveries that ultimately affect their prognosis.
Let’s talk about the research: antisense oligonucleotides
Now, 60 years from its initial characterisation, and despite a growth in knowledge, PSP remains untreatable. This is a harsh reality for those diagnosed, with an average life-expectancy after diagnosis of 5-7 years, and severe disability setting in around 3-5 years following the onset of symptoms. Nonetheless, active research is taking place to treat PSP, such as the work carried out by Dr Boyd Ghosh.
In a study led by Dr. Ghosh, which ended in September 2021, Maggie Walsh (65) was treated for PSP using antisense oligonucleotides (ASOs), a therapeutic that had never been trialled in the UK before. ASOs influence the way RNAs are used as templates for protein synthesis. For example, ASOs can bind to exon 10, causing RNA containing exon 10 to be broken down by an enzyme called RNase H. Alternatively, ASOs can bind to and block sites on the RNA where other proteins would usually bind to kickstart protein synthesis. As well as this, ASOs can be engineered to bind to specific signals that determine whether exon 10 is included or excluded in alternative splicing.
Through these numerous mechanisms, ASOs can prevent exon 10-containing RNA from being used to synthesise tau or ensure exon 10 is skipped in splicing. Both outcomes reduce the amount of 4R-tau synthesised, theoretically leading to a reduction in the symptoms of PSP. Now, only a year on from Maggie Walsh’s initial treatment, it is too early to draw conclusive results from the trial. But this work nonetheless provides promise for further investigation into the treatment of PSP and tangible hope for those with the disease.
Modifying tau
Microtubules, the structures supporting the cell skeleton, are stabilised by binding to tau. Chemical groups can be attached to amino acids, the building blocks of the tau protein, via processes such as phosphorylation and glycosylation. The balance of these modifications influences how tau binds to microtubules, and thus microtubule stability. Phosphorylation leads to neurodegeneration and microtubule destabilisation, and as we age, it is thought to become more prevalent, causing tau to bind to and stabilise microtubules less effectively, causing neurodegeneration.
Currently, the regulated addition and removal of these modifications is a point-of-interest in the treatment of PSP. For example, microtubules are stabilised most effectively by tau when tau is highly glycosylated, i.e. large amounts of sugar-type groups have been added to the protein. The sugars crowd tau’s surface, preventing the addition of other chemical modifications, such as phosphorylation. This reduction in phosphorylation causes tau to more effectively bind to and stabilise microtubules.
Thiamet-G is a proposed inhibitor of the surface-crowding glycosylation, so it could allow tau phosphorylation and microtubule stabilisation. This drug has already been shown to reduce aggregation of 4R-Tau proteins in the brains of transgenic mice. Many are hopeful that this success will translate into clinical trials and the treatment of PSP in clinical settings.
The orphan disease problem
There is a morally grey, yet undeniable truth that for a disease to be attractive to research groups and pharmaceutical companies it must fulfil a drug developer’s ideology: a clear therapeutic target, regulatory path, and large patient populations. In many ways, PSP fails to fit the bill. Its rarity means that the perceived benefits of investing in PSP research are small, and ageism in research may contribute to researching a disease largely affecting over-60s being less of a priority. This tends to deter interest and investment into PSP research.
To combat this reluctancy, the UK (together with other European countries) has adopted a common policy on orphan drugs. An “orphan disease” is one so rare that research into its treatment is often considered unprofitable. The policy provides incentives that promote research into rare diseases in a market that would otherwise avoid this.
Alongside the government-mediated incentivisation of research into PSP and other rare diseases, these diseases should themselves be considered worth investing in, at least from an ethical and scientific standpoint. Scientific research is not linear, and especially for a neurodegenerative disease such as PSP, research into the disease could reap unexpected and wider benefits.
This is because PSP is not the only tauopathy. Currently, over 26 tauopathies have been identified, from the more commonly known parkinsonism and frototemporal dementia (FTD), to lesser-known diseases such as chronic traumatic encephalopathy and dementia pugilistica. All these diseases are characterised by misfolding and aggregation of abnormal tau proteins. So, it is highly likely that any knowledge gained in understanding PSP will be beneficial in understanding other tauopathies. As well as this, understanding rare diseases tends to contribute greatly to the development of precision medicine—medicine tailored to an individual’s needs, disease presentation, and genetic makeup.
At its core, PSP is more than a research paper or a misdiagnosis. It seems unethical to consider these diseases less in need of research and funding, especially as rare diseases, as a group, are much more common. There is so much more to learn about PSP, and more attention should be directed towards understanding it better. But even the few in the UK and around the world devoting their time to unpicking the mechanisms of this disease offer a slither of hope that soon PSP will become treatable.