Yeast: what is it good for?
Well, quite a lot of things. In a talk recently given to the Oxford Synthetic Biology Society, Tom Ellis, professor of synthetic genome engineering at Imperial College London, explained how simple baker’s yeast can be utilised in the fight against global health challenges.
Baker’s yeast, or Saccharomyces cerevisiae, is a single-celled eukaryote of the fungi kingdom. Its culinary uses have been known for thousands of years, from ancient Egyptians using it to make bread to brewers and winemakers using it for fermentation. Stepping into the 20th century, yeast became a great way to produce medicines, such as insulin, thanks to its safety, fast growth rate, low cost and ability to be scaled for high-throughput production.
Scientists have looked to yeast to solve many global challenges including the production of biofuels, elimination of waste, production of materials like synthetic spider’s silk and even plant-based meat products like the Impossible™ Burger. Now, yeast is also being conscripted to fight global health challenges. And at the heart of many of these battles is Professor Ellis and his team.
Metabolic disorders
One of the biggest health problems we are facing is the increase in metabolic disorders such as diabetes. The pancreatic cells of a type 1 diabetic are dysfunctional and therefore cannot signal to other cells to raise or lower blood glucose. Professor Ellis’ lab set out to develop a system in yeast that could detect blood glucose levels but struggled to transfer the system from yeast to mammalian cells. However, from this research, the idea was born that yeast cells could be reprogrammed to detect interesting metabolites.
The receptor in yeast that detects glucose is from a family called G-protein coupled receptors (GPCRs). This is a diverse but highly conserved family of receptor proteins that recognise a wide variety of ligands. These receptors are coupled with a G protein that activates a kinase signaling cascade, leading to the movement of transcription factors into the nucleus, where they interact with promoters that direct the expression of a particular set of target genes.
Yeast have two GPCRs for the detection of two metabolites: glucose and mating pheromones. If you replace the GPCR for the mating pheromone with a GPCR for your metabolite of interest, remove the genes responsible for inhibiting cell growth and change the promoter that induces expression of specific genes, you can use your metabolite to switch on the expression of a target gene.
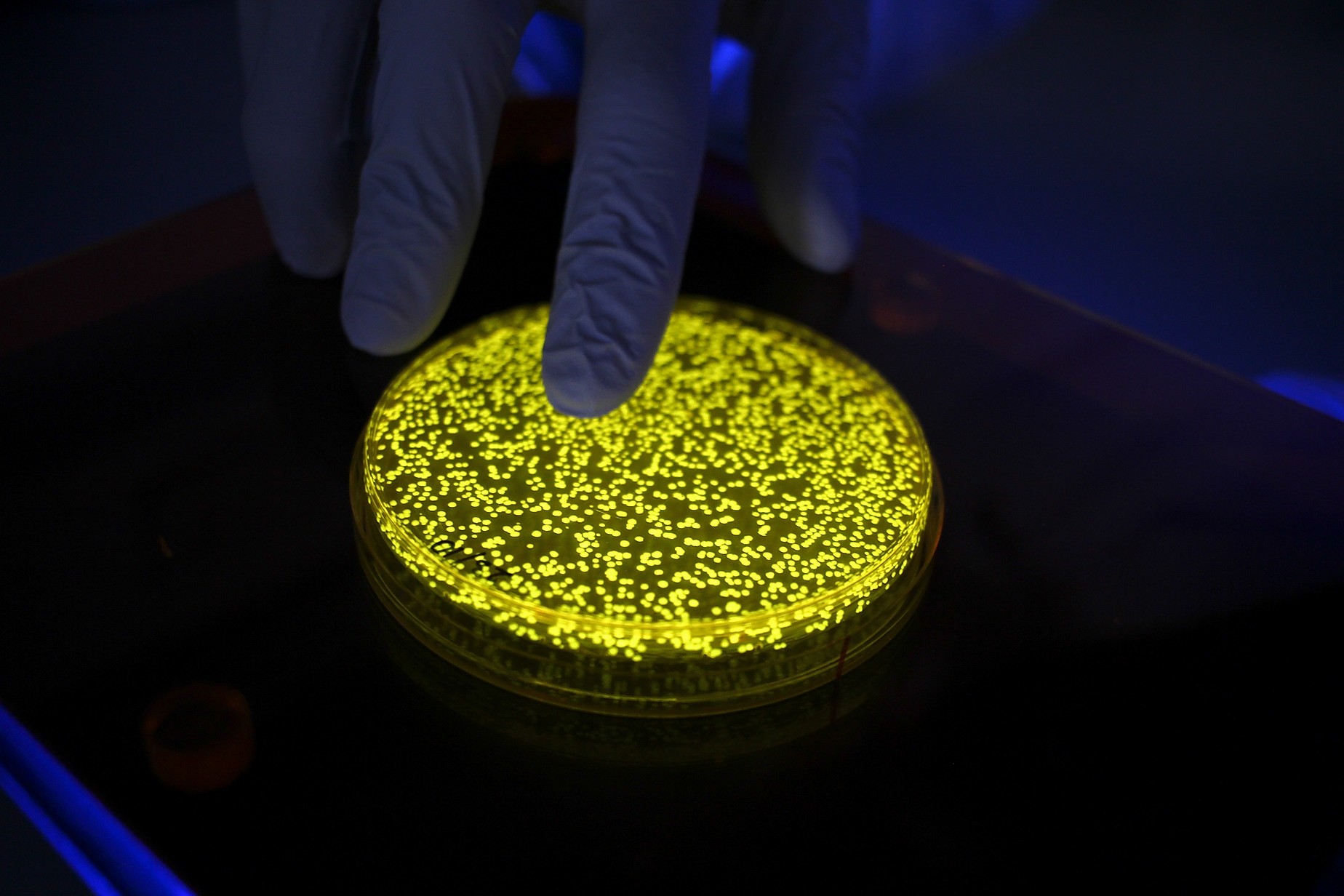
By using the promoter to switch on the expression of a reporter gene that codes for a green fluorescent protein, which would make your yeast cells glow green, you can build a system that signals when your metabolite of interest is detected. By removing the genes responsible for cell growth inhibition, you avoid triggering any secondary signaling pathways that arrest the cell cycle and maintain a stable level of cell growth.
Dr William Shaw, from the Ellis lab, took this a step further and used a CRISPR-Cas9 gene-editing system to remove an additional 13 accessory genes from the S. cerevisiae GPCR signaling pathway. These refactored yeast cells possess a much more stream-lined version of the signaling cascade, preventing any unnecessary side reactions from occurring that would inhibit cell growth or divert resources from the target pathway.
In addition to stable growth, minimal gene expression also comes with the benefit of being much easier to model mathematically. By modelling different protein expression levels within the signaling pathway, the detection system can be quickly fine-tuned to produce the optimum detection system for the metabolite. The robustness of the process was proved when the lab could produce systems to detect two human metabolites, adenosine and melatonin, from scratch in just one week. Shaw’s refactored S. cerevisiae cells were shown to be as sensitive as a mass spectrometer in the detection of melatonin, and these cells are being used to detect melatonin in blood samples for a sleep disorder experiment.
Antimicrobial resistance
Antimicrobial resistance is also a huge threat to global health. Yeast can be used to detect the presence of dangerous pathogens and also help us make new antibiotics to fight them.
Yeast and other fungi are often overlooked microbes, with so much attention directed towards bacteria. S. cerevisiae is harmless to humans but, in the same way that bacterial species can be friendly or unfriendly, certain species of yeast cause disease as well. Candida albicans and Candida auris are two pathogenic strains of yeast that have caused major outbreaks in hospitals around the world. Quick identification of cases is crucial to prevent outbreaks occurring. Shaw’s refactored yeast cells were able to detect mating pheromones produced by different fungal pathogens with picomolar sensitivities.
The Ellis lab’s Dr Ali Awan has modified yeast to produce benzyl-penicillin by taking the genes from the Penicillium mold that naturally produces the antibiotic and inserting them into the yeast genome. The speed and scalability of growing yeast allowed Awan to test over 1000 different variants with varying levels of gene expression to select the one that produced the most penicillin.
The same approach was used by Glen Gowers in the Ellis lab to produce the antiretroviral substance, betulinic acid. By changing the genes involved in the biosynthesis pathways for these compounds, you could alter the antibiotic produced and generate new potential antibiotics on a high-throughput scale.
Viral pandemics
The final global health challenge being tackled by yeast is viral pandemics. Yeast is playing a huge role in fighting SARS-CoV-2, and not just for everyone’s new-found sourdough hobby!
To study SARS-CoV-2 scientists need to produce the viral DNA and RNA in the lab. This is usually done by growing the virus and purifying its genomic material. Pandemic viruses like SARS-CoV-2, however, are tightly controlled and only certain labs are granted access to work with them.
Researchers at the University of Bern have found a solution that avoids working with the dangerous virus. By introducing the viral genes into yeast, they engineered the cells to produce copies of the viral DNA which they could then use to study SARS-CoV-2. The expression of SARS-CoV-2 genes in yeast also enables scientists to test huge libraries of drugs on the yeast cells to identify novel therapies that target the SARS-CoV-2 proteins.
In addition to antibiotics, vaccines can also be produced on a large-scale using yeast. Professor Xiao-Ning Xu, also of Imperial College London, is producing a SARS-CoV-2 vaccine using virus-like particles (VLPs). These are spherical particles made of structural proteins fused with viral antigens, the proteins found on the surface of viruses that we produce immunity against. Yeast is being used to produce the SARS-CoV-2 ‘spike protein’ antigen on a large scale to assemble into VLPs.
If a vaccine proves safe and effective, production using yeast could be scaled enormously to make millions of VLPs quickly and cheaply. Additionally, as S. cerevisiae is not toxic for humans, production of the vaccine in yeast is much safer than previous methods using bacteria.
Professor Ellis highlighted that in the fight against global health challenges it is becoming rapidly obvious just how crucial a role yeast can play. From diabetes to viral pandemics, this simple microbe really can do it all.
Tom Ellis is leading a research team in synthetic genome engineering and synthetic biology in the Department of Bioengineering. His research focuses on developing the foundational tools for accelerating, automating and scaling design-led synthetic genomics and synthetic biology, focusing on research projects in yeast (S. cerevisiae) as well as applied projects in other industrially-relevant and medically-relevant microbes.
Title image from https://www.tomellislab.com/our-research?lightbox=dataItem-jtzsclvh1