When cystic fibrosis was first identified in 1938, a diagnosis at birth was almost a death sentence, with a life expectancy of six months [1]. Yet, with improved diagnosis and treatments, nowadays half of the patients live into their 40s and beyond [2]. In recent years, the shift from symptomatic treatment to precision medicines has been revolutionary for patient life expectancy. Moreover, early-stage studies using antisense oligonucleotides—short molecules that can increase levels of specific proteins—hold potential for treating rare forms of cystic fibrosis for which current therapies are unsuccessful [3].
The disease
Cystic fibrosis is a recessive genetic condition, so sufferers must receive faulty genes from both parents to inherit the disease [2]. For the 10,000 cystic fibrosis patients in the UK, the condition is life changing. Yet it is caused by mutations in a single gene: the cystic fibrosis transmembrane conductance regulator (CFTR) gene [4]. In healthy subjects, the CFTR gene codes for the CFTR protein, a chloride ion channel. Channel proteins are a special type of protein that are embedded in the cell surface membrane. They allow the passage of substances in and out of the cell through their hollow structure. For the CFTR protein, it specifically permits chloride ions to exit the cell. Once outside the cell, chloride ions attract water to maintain the osmotic balance, i.e., so the outside environment does not become too salty and concentrated [5].
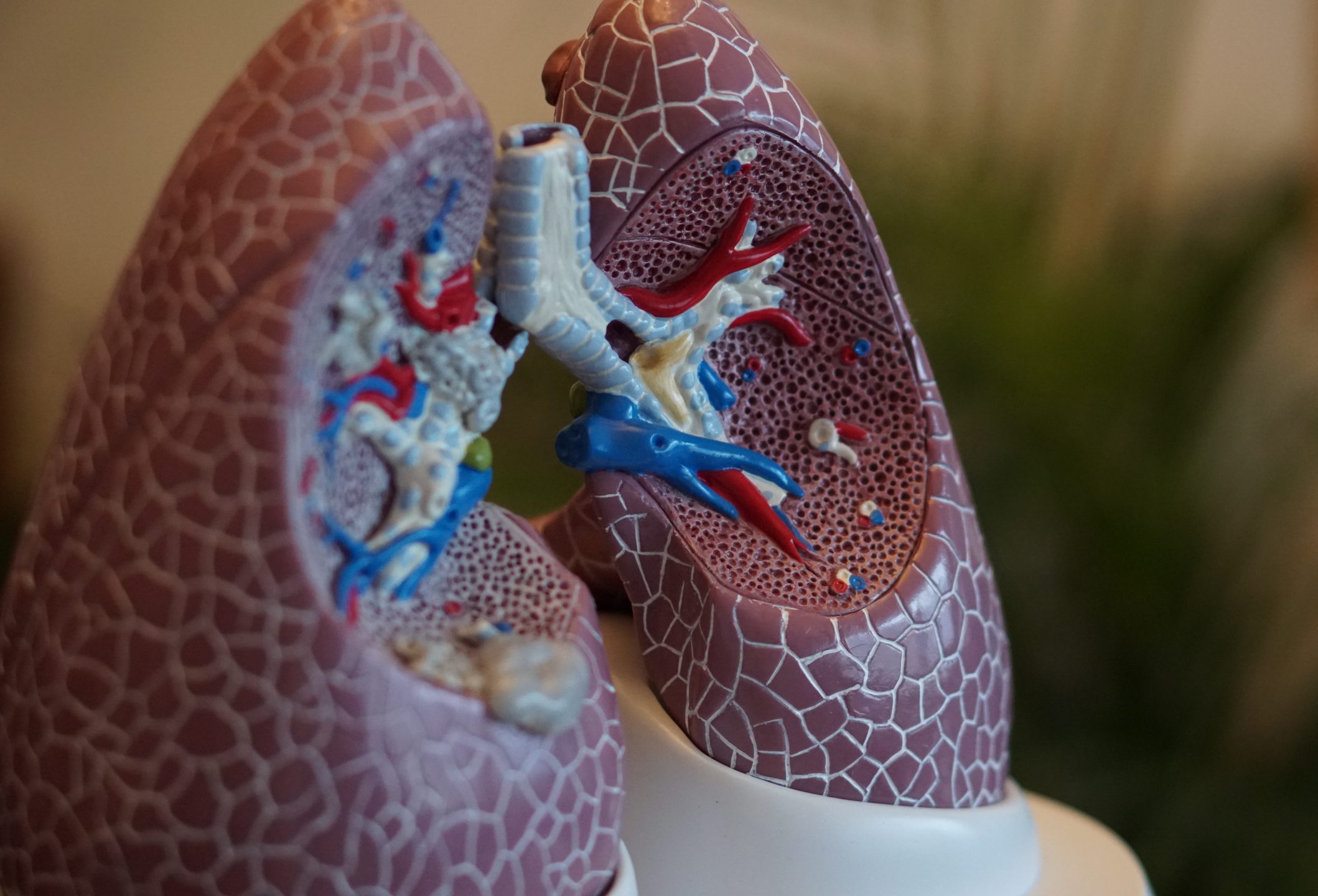
In cystic fibrosis patients, the CFTR gene is mutated so a non-functional CFTR channel protein is produced. Thus, chloride ions cannot flow out through the channel, so less water moves to the outside environment as well. This has major effects on the mucus that lines tracts in the body, such as in the lungs and the digestive system, where it becomes thick and sticky. The sticky mucus in the lungs cannot be wafted up by tiny hairs lining the airways and is not coughed out.
Aside from giving breathing difficulties, any pathogens caught in the mucus become stuck in the lungs. In cystic fibrosis patients this leads to recurring chest infections and, over time, to lung damage, the main cause of death for patients [5].
In the digestive system, the pancreas releases most of the enzymes we need to break down food and absorb nutrients. Nonetheless, sticky mucus can block pancreatic tubes and prevent enzymes being transported to the small intestine where they act on food. As a result, cystic fibrosis patients struggle to absorb nutrients from food and can suffer from malnutrition. Patients can also develop cystic fibrosis-related diabetes as the pancreas releases insufficient insulin (a hormone that regulates blood glucose levels, deficiently acting in diabetics) due to scarring caused by the mucus [6].
The limited options
Before the molecular mechanisms behind cystic fibrosis were understood, treatments were restricted to easing symptoms. This could include providing antibiotics to treat chest infections, using medicines and breathing devices to help clear the lungs, and taking enzyme supplements to avoid malnutrition [7]. As a last resort, patients with poorly-functioning lungs could receive a lung transplant, but the waiting list is long (18-months on average), the operation is risky, and the faulty CFTR protein remains in other organs of the body where treatment will still be needed [8]. These symptomatic treatments provided a limited improvement in patient quality of life as they could not tackle the root cause of the condition: the CFTR protein.
Although all cystic fibrosis patients have a mutation in the same CFTR gene, over 2,000 mutations have been identified. To simplify choosing personalised medicines for patients, the mutations have been sorted into six classes, depending on their effect on the CFTR protein.
Class I mutations encode for a shortened CFTR protein, which is prevented from being produced. In Class II, the CFTR protein is not transported to the membrane (for example, because it does not fold correctly so is prematurely degraded). In Class III, the CFTR channel doesn’t open properly due to a faulty gating mechanism (the hollow channel protein has a gate at the end that can be opened and closed to control passage through it). For Class IV, the CFTR channel is misshapen so chloride ions cannot pass through as easily as in healthy cells. Class V mutations produce a lesser amount of CFTR protein than needed. Finally, in Class VI, the CFTR protein produced is less stable so has a shorter lifespan in the cell membrane before being naturally degraded [9, 10].
Identifying the specific class of mutation a patient has is vital for choosing an appropriate therapy. For example, it would be pointless giving a Class III cystic fibrosis patient (with a gating defect) a drug to help traffic the CFTR protein to the membrane, as this will not open the CFTR channel so chloride ions still wouldn’t be able to leave the cell [9].
The revolution
Several novel drug therapies for cystic fibrosis have been developed in the past decade. In December 2016, the NHS started using ivacaftor, the first medicine specifically targeting the CFTR protein, as opposed to non-specifically easing symptoms [11]. Ivacaftor (brand name Kalydeco) is a drug that holds the CFTR channel gate open so is used in treating Class III gating mutations [12, 13]. This was a major breakthrough for cystic fibrosis research; however, it could only be used on a small proportion of patients as 85% of cases have a Class II mutation instead, where the CFTR protein is not successfully trafficked to the membrane. Most cystic fibrosis patients have the F508del mutation, categorised as Class II [9].
After the development of the ‘potentiator’ (to hold the gate open) ivacaftor, the next step was to produce a ‘corrector’ to aid the CFTR protein folding into the correct shape so that it can be trafficked to the cell membrane [14]. When clinical trials began for F508del patients (Class II trafficking to membrane defect), it was expected that providing a corrector would recover CFTR protein function as the channel protein would reach the cell membrane where it could allow chloride ion passage. Surprisingly, this did not occur. Once in the membrane, the CFTR protein exhibited Class III (gating) and IV (poor chloride transport through channel) mutant characteristics, aside from its assigned Class II. To observe patient benefits, a potentiator was also required to hold the CFTR channel gate open once it had been embedded into the cell surface membrane. Thus, combination treatments were developed [10].
A number of correctors have been released for use in combination with the potentiator ivacaftor. These therapies include: Symkevi (ivacaftor and tezacaftor), Orkambi (ivacaftor and lumacaftor) and Kaftrio (ivacaftor, tezacaftor and elexacactor) [15, 16, 17]. The triple-combination therapy Kaftrio was most recently released on the NHS in August 2020, and has seen the greatest patient benefits thus far from cystic fibrosis treatments [18, 19].
The revolution continues
Kaftrio and other combination therapies have been life-changing for many cystic fibrosis patients. But, for those with rarer forms of the condition there is still a need for novel treatments. For instance, Class I mutations encode for a shortened CFTR protein which has reduced function. Yet, the larger issue is that the cell prevents the attenuated protein from being produced altogether. The cell recognises the shortened length of the intermediate product, mRNA (a mobile copy of the gene, used as a template for protein synthesis), and flags it as harmful so the mRNA is degraded before it can instruct CFTR protein production. Thus, the shortened but slightly functioning CFTR protein cannot be produced [20].
Unfortunately, supplementing a corrector and potentiator (to traffic the CFTR channel protein to the membrane, and to keep the channel open), such as in Kaftrio, is ineffective for these mutations because there is not enough protein product remaining in the cell for protein function to be recovered. Hence, a different approach must be taken [3].
Antisense oligonucleotides (ASOs) are short, single-stranded pieces of DNA or RNA that have been used in recent studies to override the cell’s mechanism of degrading the shortened mRNA for the CFTR protein. The ASOs can recognise and bind specifically to the mRNA to prevent it being flagged by the cell. As a result, the mRNA is not degraded, so it can instruct the production of CFTR protein. Although the shortened CFTR protein produced only has partial function, it’s an improvement on having almost no CFTR protein, as is without ASO treatment. As this is such a new therapy, trials using antisense oligonucleotides for cystic fibrosis treatment have so far only been tested on cell lines. Yet, the results were promising and in years to come they may be a revolutionary treatment for cystic fibrosis patients [3].
In summary, cystic fibrosis treatment has massively improved over the past decade with the development of combination therapies, such as Kaftrio, to tackle the lack of functional CFTR protein expressed in patients. For those with rarer and often more severe forms of cystic fibrosis there is currently a lack of precision medicine to target the CFTR channel protein; however, early-stage antisense oligonucleotides trials hold potential. With improved CFTR function, chloride ions can exit cells, attract water, and reduce the level of sticky mucus that has detrimental effects on respiratory and digestive systems, altogether improving patient quality of life.