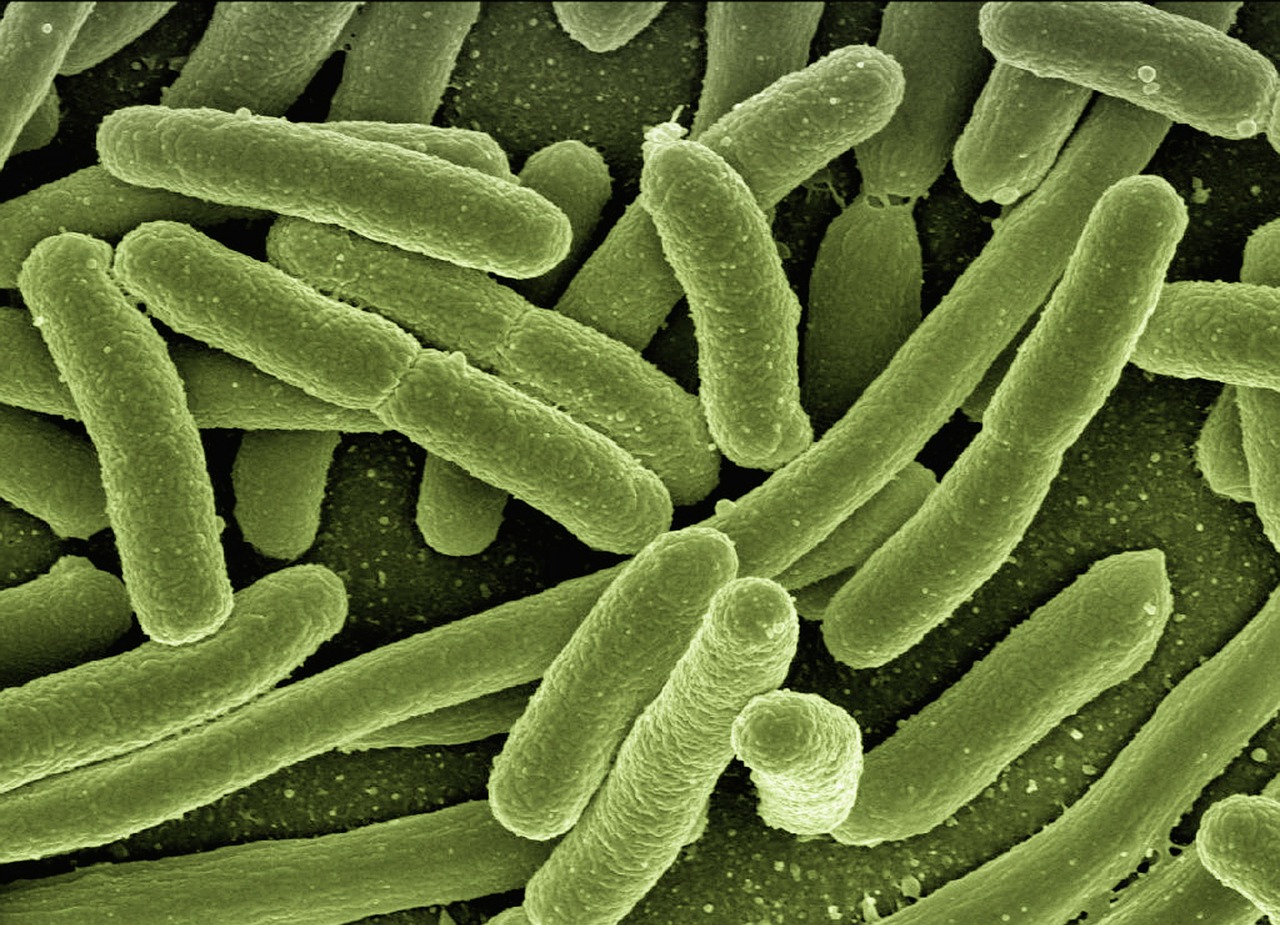
Tuberculosis is currently the most deadly infectious disease worldwide, killing an estimated 1.7 million people in 2016. The only licensed vaccine currently available is BCG, which is only 70% effective. While most vaccines work by inducing antibodies, mycobacterium tuberculosis (or Mtb for short) hides inside cells, preventing antibodies from reaching it. T cells, which help kill intracellular pathogens, seem to be much more important for protection against tuberculosis. Conventional T cells have hugely diverse receptors which bind pathogen peptides presented on MHC molecules, causing the T cells to differentiate and divide.
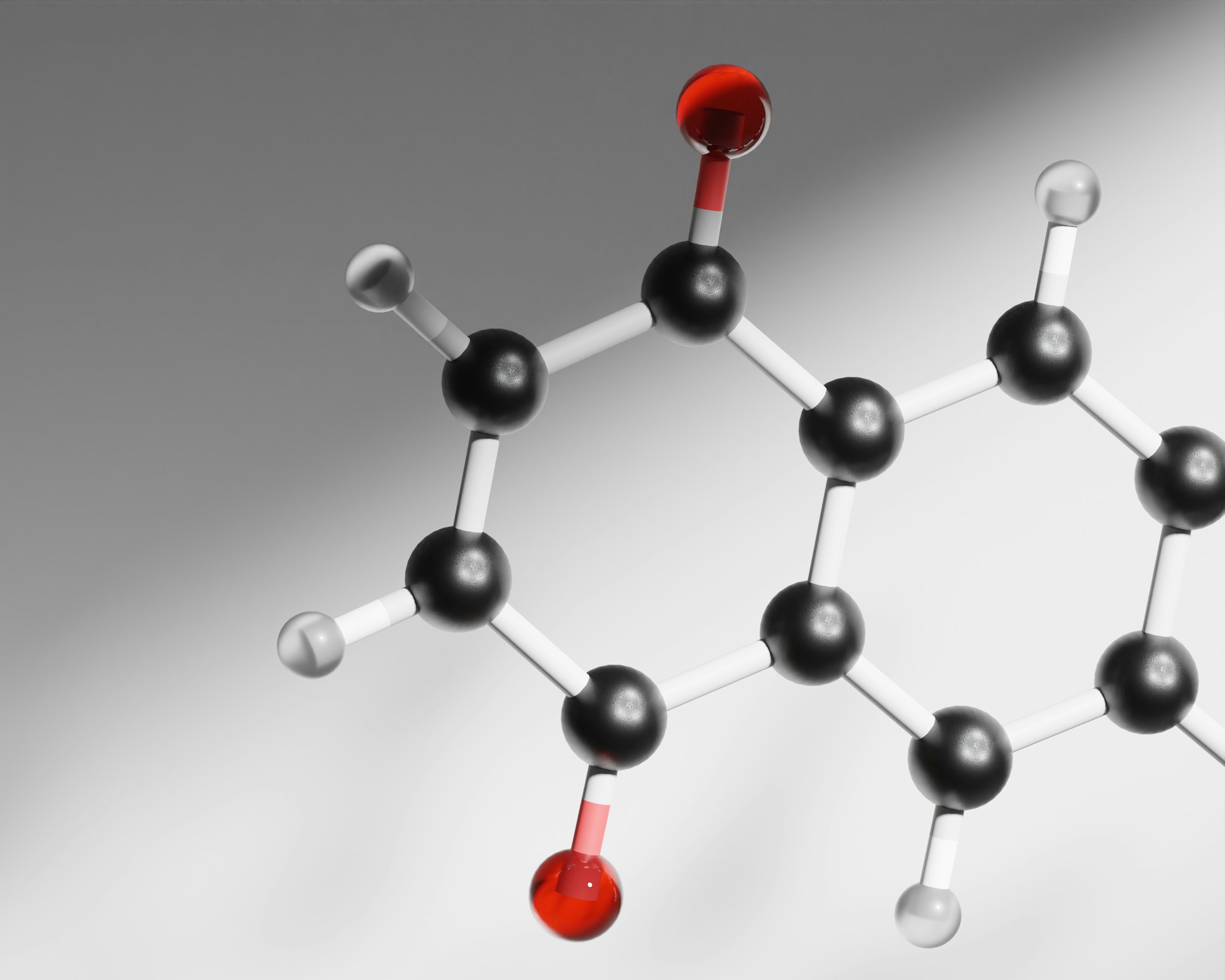
Unlike most bacteria, Mtb has a waxy coat containing lipids known as mycolates. Mycolates are presented by CD1 rather than MHC molecules, binding to conserved receptors on germline-encoded mycolyl lipid reactive (GEM) T cells, an unconventional T cell subset discovered only four years ago. In a recent study by the universities of Southampton and Bangor, researchers found that CD1b was present in the lungs of tuberculosis patients, suggesting these cells could play a role in the immune response to Mtb. As different Mtb strains produce mycolates with slightly different structures, understanding how these lipids bind receptors will be necessary to develop novel anti-TB vaccines targeting GEM T cells. By adding different mycolates to cells expressing GEM T cell receptors, the researchers found that the “head” of the lipid wasn’t important for specificity, while the “tail” was, affecting how strongly T cells were activated. Thus by manipulating the chemical structure of the mycolate tail, future vaccines could be optimised to maximise the GEM T cell response, hopefully improving efficacy.