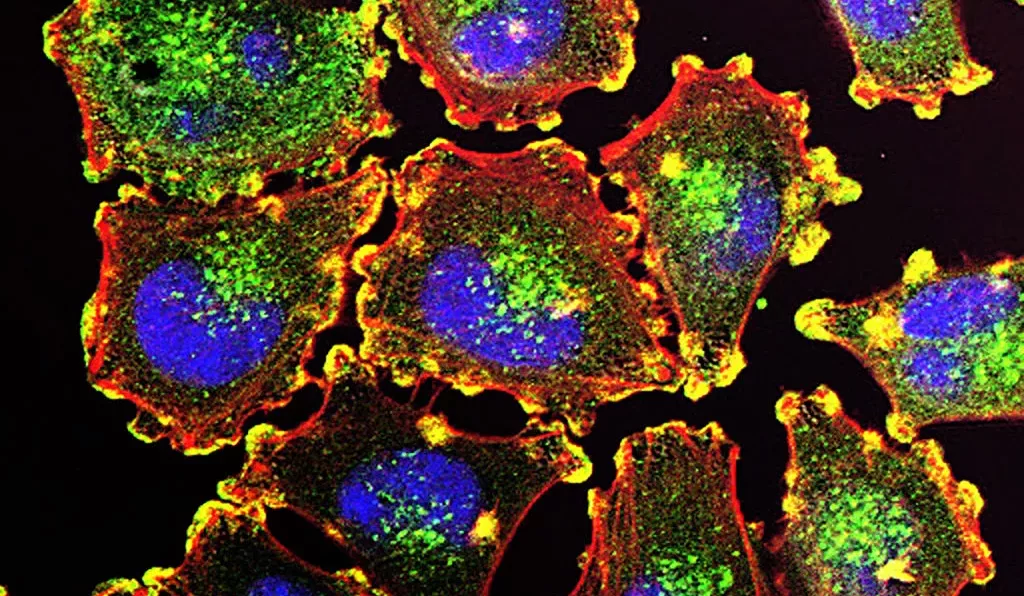
Metastatic melanoma cells imaged to show the structures that enable them to move. The morphology of such cells was investigated in the study reported here. Image credit: Julio C. Valencia, public domain, via Wikimedia Commons. Originally exhibited through the 2015 Cancer Close Up project by the National Cancer Institute (US).
A new paper published in Science Advances by a research group at the Institute of Cancer Research, London, has provided new evidence for using the size of cancer cells to direct treatment strategy. The group, led by Chris Bakal, Professor of Cancer Morphodynamics, investigated the morphology and chemistry of melanoma cells (skin cancer).
Using proteomic and image analysis techniques, it was found that specific mutations gave rise to tumours with either small, medium, or large cells. The concept of cell size uniformity amongst cells of the same type within a tissue is well established. In addition, the size of cells can have important consequences for their function—from impacting the amount of a specific protein in the cell to affecting how nutrients are obtained.
The cells used in the reported experiment contained two of the most common mutations driving skin cancer, in the genes for the enzymes N-Ras (NRAS) and B-Raf (BRAF). Both of these proteins are important in signalling to cells to divide, with their mutant forms driving the rapid and uncontrolled cell division seen in tumours. NRAS cells tended to be on the larger side, whereas BRAF cells were much smaller.
Why and how cancer cells achieve this size diversity is unknown. Notably, quantifiers of cell morphology in this study could be directly correlated with a different protein make-up of the cell. Smaller cells displayed a higher concentration of proteins involved in the DNA damage response, indicating they could be particularly vulnerable to therapeutic agents targeting DNA repair proteins such as PARP inhibitors.
These drugs work to kill cancer cells by preventing them from repairing broken DNA, with the accumulation of damage eventually eliminating these cells from the population. In contrast to the protein composition of small cells, larger cells displayed greater signs of inflammation, showing potential for the use of immunotherapies across tumours composed of cells of a larger size.
“Cell size could matter more than we thought in the development of personalised cancer medicine”
Although cancer may be described as a single disease, it encompasses a vast diversity of cell types and gene mutations—as a result, the response of different patients to the same treatment can vary hugely. This has motivated research into more personalised therapies in recent years, where researchers have attempted to identify features of cancer cells that make them more susceptible to specific treatments.
Combined with the fact that commonly used chemotherapies are often associated with significant side effects and an increased risk of developing other tumours, optimising the anti-cancer effect of any drugs given to patients is essential.
This study therefore provides an important insight into how size could matter more than we thought in the development of personalised cancer medicine. If similar conclusions are made from studies on other cancer types, a simple analysis of what cancer cell appearance, rather that complex investigations into their genome, could help clinicians devise the most beneficial treatment plan for patients.