by Patrick Brown, Year 12, Merchant Taylors’ School Northwood, Middlesex.
Seventeen million people were diagnosed with cancer in 2018. It is a major killer, caused by the accumulation of mutations in DNA. Billions of pounds have been invested into cancer research and cancer treatments, but the complexity of cancer and its variations has meant that existing treatments such as chemotherapy and radiotherapy are not always successful. A new “living medicine” called CAR T-cell therapy or chimeric antigen receptor therapy, takes a different approach on tackling cancer, by using and modifying the patient’s own cells to fight cancer. This treatment is providing hope for cancer patients where all other treatments have been exhausted and it is hoped that CAR T-cell therapy will become a mainstream treatment for cancer in the future.
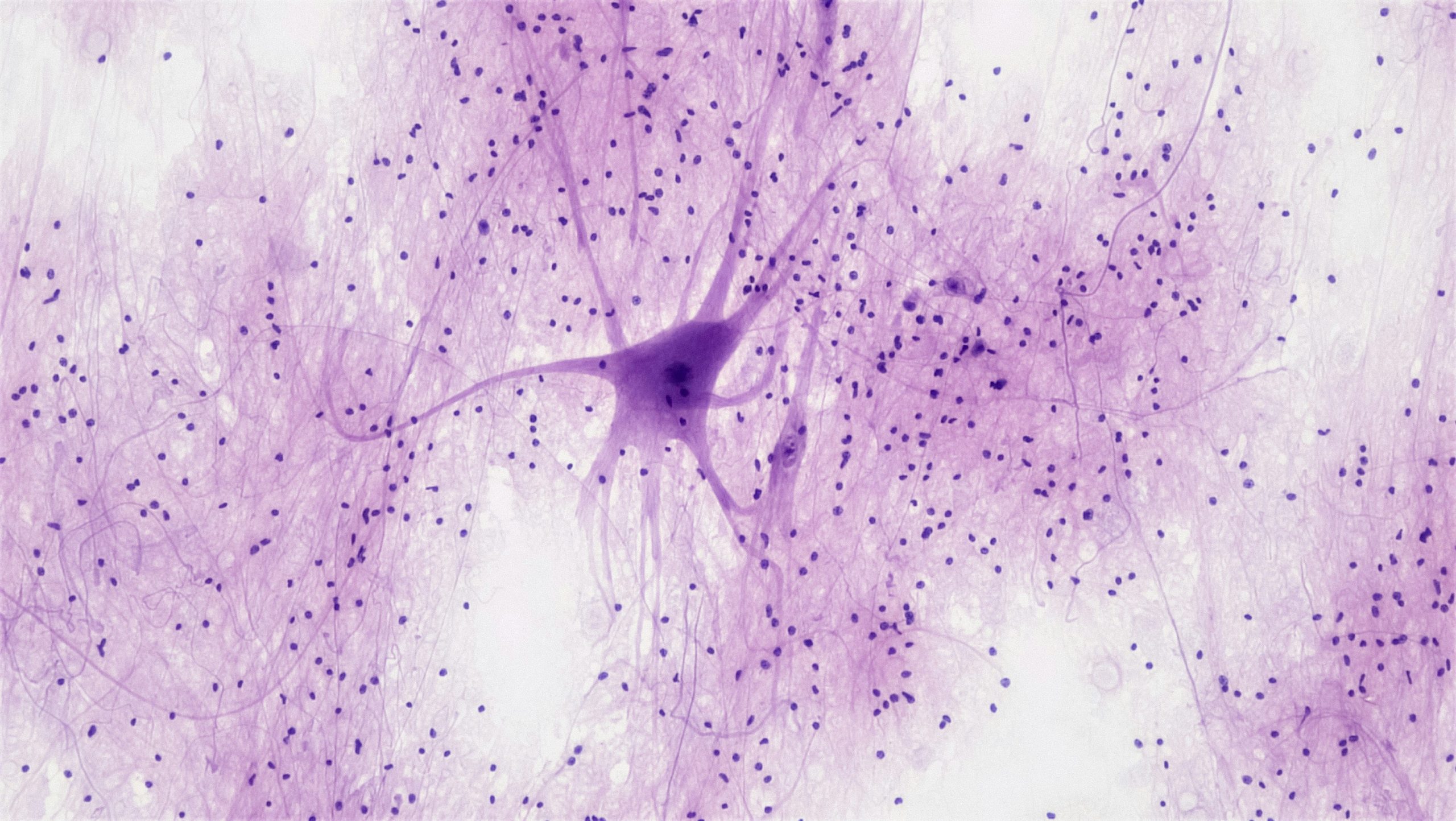
CAR T-cell therapy works by reengineering T-cells. They play a central role in the immune response and they actively scan the body looking for foreign cells. Every cell in the body is identified by peptide-HLA complexes, which stick out on the surface of cells and act like a ‘barcode’. They are commonly known as antigens. In order for T-cells to scan a cell, they must bind to it. How well and for how long the T-cell receptor binds to the antigen, determines whether the T-cell will kill the cell by releasing chemicals, or move onto to other cells.
T-cells normally work well in the identification of foreign cells. However, the binding of naturally occurring T-cell receptors to cancer cells, tends to be poor. This is because cancer proteins appear very similar to naturally occurring proteins and are good at evading the immune system. A process called thymic selection exists to prevent the immune system attacking itself, resulting in an autoimmune disease. Any T-cell receptor that recognised the self-proteins strongly, would have been deleted during the thymic selection process, so any remaining T-cells do so weakly. It is a result of this process that T-cells generally fail to recognise and kill cancer cells. In addition, cancer cells express a lower number of antigens, which further decreases the chance of recognition by a T-cell.
CAR T-cell therapy is a treatment designed to overcome this issue, by genetically modifying the patient’s own T-cells to specifically recognise a certain antigen associated with their cancer. It is a personalised treatment unique to the patient and allows the immune system to identify cancer cells and trigger an immune response. It begins by removing the patient’s T-cells during a process called leukapheresis. Like dialysis, it filters the blood, but instead of removing waste products and excess fluid, it removes T-cells. The T-cells are then frozen to preserve cell integrity and sent to a laboratory. Here, the T-cells are thawed and re-engineered using a disabled virus to genetically encode the cells. The T-cells now recognise the specific antigens of a cancerous cell such as CD-19, an antigen commonly found in leukaemia (blood cancer) cells. The modified T-cells are then multiplied, washed and undergo a strict quality check, before being frozen again and sent back to the patient. The re-engineered cells are now intravenously inserted back into the patient’s blood. Once inside, the T-cells continue to multiply and begin to destroy cancer cells expressing the specific antigen.
CAR T-cell therapy has been rapidly advancing in recent years, with approval by the NHS in October 2018. It is now available to patients who have not responded well to other forms of treatment. The therapy is now in its second version, with many of the severe side effects, such as cytokine release syndrome (a condition where there is a large, rapid release of cytokines from immune cells affected by the treatment), being suppressed significantly. Nevertheless, it remains an extremely intensive process. Due to the personal nature of the treatment, the cost can be upwards of £200,000 per patient and there is no guarantee it will work.
Currently this treatment is used to treat different types of lymphoma and leukaemia. In the future, scientists hope to be able to improve the efficiency of the delivery of CAR T-cell therapy by eliminating the need for the patient’s own T-cells. Like blood, it is hoped that people will be able to donate T-cells that can then be re-engineered and given to many patients.