Night shift workers may be more likely to develop diabetes than their regular 9–5 working counterparts.
The proposed reason for this correlation lies in the disruption of circadian rhythms. These are changes in the body that follow a 24-hour cycle, such as body temperature (lower at night than in the day) and the release of hormones (like the sleep hormone melatonin, which is released at night).
Circadian rhythms are aligned with the external time. This means that if your daily routine contradicts the environmental time, your circadian rhythms get confused. This can have drastic health consequences, such as an increased risk of developing diabetes, hypertension, and coronary heart disease.
How the body knows the time
Internal timekeeping is a job designated to the brain. The brain relies on signals from the eye’s retina where a specific type of neuron—a photosensitive ganglion cell—detects light levels.
When the eyes are exposed to light in the morning, the retinal neurons send a nervous signal to the hypothalamus in the brain. Within the hypothalamus, there is a group of around 20,000 neurons collectively known as the “suprachiasmatic nuclei” (SCN) that receive the light information from the eye. This synchronises the circadian rhythms for the entire body.
So, when it’s light outside, the body knows it’s morning and prepares for the day ahead.
The SCN uses both nervous and hormonal signals for communicating the time of day to all other cells in the body.
A key example of this is the use of the hormone melatonin for indicating night-time. When it gets darker at night, these specialised neurons in the retina communicate the time to the SCN in the brain.
Then, the SCN signals to the pineal gland (also within the brain) to trigger its release of melatonin, commonly named the sleep hormone. Finally, melatonin travels through the bloodstream and communicates with cells throughout the body to make you feel more tired and ready for sleep.
Although light is the primary means by which the body synchronises its internal circadian rhythms with the outside environment, there are also non-photic factors such as food, exercise, and social cues that can have a small influence on our body clock.
How individual cells in the body follow the time
The SCN is the central coordinator of circadian rhythms in the body but, in fact, all cells have their own internal clock that runs for roughly 24 hours. The purpose of the SCN is purely to synchronise these internal clocks because cells quickly become misaligned from each other if left alone without central control.
It is important that cells are synchronised so that they can work together to perform biological tasks at the right time of the day—it would be counterproductive if some cells were getting ready for the busy day ahead while others were preparing for the body to sleep.
Within individual cells, circadian rhythms are controlled using a negative feedback loop of gene expression.
In essence, genes code for proteins, and all our cells (except in the germline, i.e., egg and sperm cells) each contain our complete set of genes. But not all proteins are needed in every cell. There is little use for a nerve cell in the brain to produce enzymes that digest food in the stomach or small intestine.
Cells have evolved mechanisms to regulate gene expression (i.e., how much protein will be synthesised from its gene at a given time) in response to stimuli or cell type and location in the body, so genes can be turned on or turned off.
The cells’ internal clock is governed by the relative levels of two antagonistic groups of proteins, all synthesised from various “CLOCK” genes. These two groups of CLOCK proteins include a positive arm and a negative arm, which interact with each other in a delayed negative feedback loop.
When the SCN sends out a signal that it is the morning, cells initiate expression of the positive arm of CLOCK genes. Once produced, the positive CLOCK proteins promote expression of the second group of CLOCK proteins—the negative arm.
Once the negative CLOCK proteins have been synthesised, they inhibit the positive CLOCK proteins. This negates the positive CLOCK proteins’ up-regulatory effect so the negative CLOCK proteins are no longer synthesised and will naturally degrade.
As the negative CLOCK proteins reduce in number, their inhibitory effect on the positive CLOCK proteins is released, and the cycle restarts itself. The entire feedback loop takes 24 hours, from the initial expression of the positive arm until their expression is stimulated for the second time.
Signals from the SCN ensure that all cells start the cycles at the same time. As such, in the morning the positive arm of CLOCK proteins will be synthesised, and these will trigger downstream pathways appropriate to the time, such as the release of hormones from the pancreas.
Throughout the day, the relative concentrations of the two groups of CLOCK proteins inform the cell of the time so that it can perform time-appropriate responses.
How circadian rhythms influence the pancreas
Amongst other roles, the pancreas is responsible for regulating blood glucose concentration.
High levels of glucose in the blood triggers the release of insulin from beta-cells in the pancreas. Insulin travels through the bloodstream and stimulates the uptake of glucose into cells for use in metabolic activities. Thus, insulin lowers blood glucose levels.
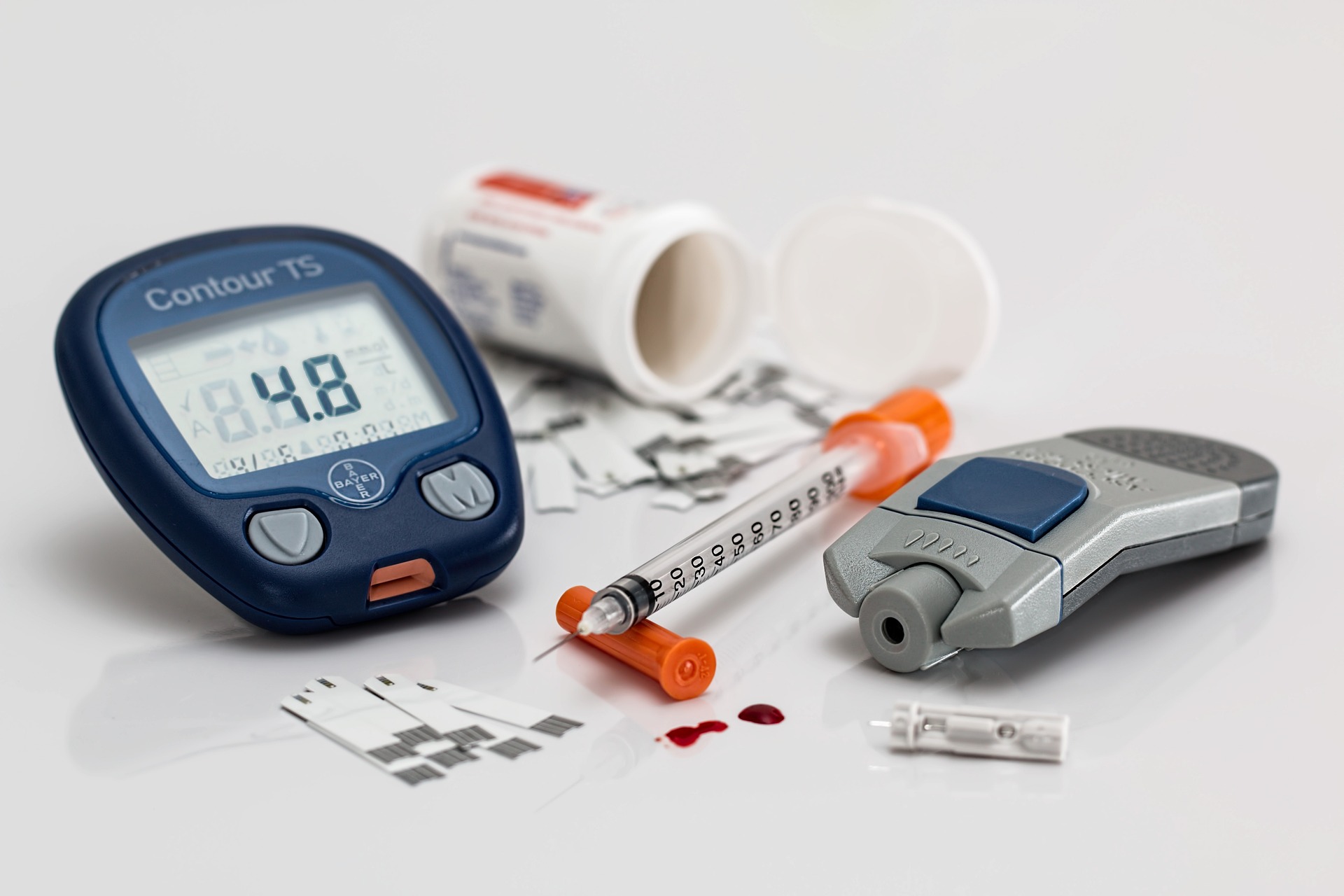
In diabetic patients, the insulin secreted from the pancreas is insufficient to control blood glucose levels, leading to hyperglycaemia (high blood glucose). Hence, diabetes can be treated with insulin supplements at specific times to control the increased glucose levels following mealtimes.
Several genetic knock-out studies have investigated the effect of CLOCK gene mutations on mice glucose and insulin metabolism.
In these studies, the CLOCK genes are “knocked out” to make them inactive, meaning that no functional CLOCK proteins can be synthesised. Any significant functional variation between knock-out mice and control mice (which have functional CLOCK genes) can then be related to the CLOCK genes, as that is the only difference between the two groups.
Such studies have demonstrated that CLOCK gene knock-out mice show impaired insulin release in response to glucose stimulation—a characteristic of diabetes. When the mouse pancreatic cells were analysed, the dysfunction was found to be in the insulin secretory pathways, not in the production of insulin.
So, circadian CLOCK genes/proteins are thought to be involved in triggering the secretion of insulin from beta-cells in response to glucose.
In human studies, naturally-found genetic variants (single nucleotide polymorphisms, known as SNPs) in CLOCK genes have been associated with an increased risk of diabetes. Combined with the evidence from mouse knock-out studies, this further highlights the role of circadian rhythms in impaired insulin secretion and developing diabetes.
This could explain why night shift workers—who have disrupted circadian rhythms—are more likely to develop diabetes than those on a regular daytime working schedule.
The link between circadian rhythms and insulin metabolism offers a potential target for diabetes research. But there are many factors not described here that are involved in such complex pathways. For example, sleep deprivation can also increase the risk of developing diabetes.
Although maintaining a regular, night-time-aligned sleep pattern is unlikely to be as effective as insulin supplements for treating diabetes, CLOCK genes hold the potential for further research into diabetes treatment. Next, studies need to investigate whether gene therapy on diabetic patient-derived cells relieves symptoms of diabetes or not.