Atreyi Chakrabarty in conversation with your brain.
In 2006, the first paralysis patient could control a computer cursor using just her thoughts and a brain-computer interface. In 2012, two more paralysis patients were able to control an independent robotic arm to grab a drink from a water bottle. Reading the brain’s electrical signals was an impressive feat, but no computer could yet directly influence the brain. Today, as we still grapple with understanding the 1.4kg gelatinous mass inside our heads, Professor Newton Howard of Oxford may have cracked its code.
Howard, an ex-lieutenant of the American security services, was compelled to understand the language of the brain when he suffered a traumatic brain injury. Through his interdisciplinary research and collaborations in mathematics, natural language processing, and computational neuroscience, Howard proposed a theoretical framework drawing from mathematics, called the Fundamental Code Unit (FCU), as a way of deciphering the brain’s activity. Using this code, he and his team are now developing a device to be able to modify activity in dysfunctional regions of the brain.
‘Think of [the FCU] as Morse code – with Morse code, you are able to express a compelling amount of information using a very basic code’, Howard explains. The FCU uses what is known in mathematics as unary code, such that for example 110 represents the number 3, and 11110 represents the number 5 and so on. Similarly, in Howard’s FCU, when a single neuron generates electrical pulses, the number of pulses, their duration, the intervals between them all result in a unary code, for example 11110. The unary code is transferred to another neuron, whose activity is then directed spatially. So for this instance a neuron receives this signal and says, “okay your job is done, I’m going to neuron number 5 next to you” and so forth. ‘We essentially will be able to read from a specific neuronal circuit and manipulate specific neurons that are dysfunctioning and allow them to be re-coded to carry out their job’, says Howard.
The final version of Howard’s implant chip, referred to as the KIWI (Kinetic Intelligent Wireless Implant), is designed to be a tiny 1.2 by 2.2 millimetres, roughly the size of a grain of rice. It will have an astounding 1 million channels, made of materials such as carbon nanotubes, enabling them to connect to surrounding neurons very precisely and operate at a higher resolution than current implants. Compared to Elon Musk’s Neuralink device, which is the size of a coin, has 1024 hair-like channels, and connects to large populations of neurons all at once, the KIWI device has 1000 times greater precision in communicating with specific neurons in a circuit.
The KIWI chip would be especially useful for individuals with neural deficits such as Parkinson’s Disease patients, whose deficits occur due to a degeneration of neurons that produce the neurotransmitter dopamine, which gives rise to the characteristic motor deficits such as tremors and progressive loss of cognition. The lack of dopamine means that surviving non-dopaminergic neurons cannot be modulated and become over-active. ‘[The KIWI chip] is directed to be placed in the areas where neurons are not working’, Howard explains. ‘It reads the activity…understands what this information means in relation to the FCU, and reconstructs [these] “modulation recipes” in the form of very small micro-volt currents’. These currents would stimulate the remaining healthy dopamine neurons to increase the levels of dopamine; ‘like a train junction…[it] bypasses the damaged neurons to relay information to the healthy ones’. This strategy is based on the principles of deep brain stimulation, which involves using electrodes to activate dysfunctional brain regions in the hope that some of the functioning neurons take over control.
But what about Parkinson’s patients who don’t have dopamine releasing neurons left? Howard stated that ‘the KIWI chip has 3 therapeutic modalities. One is neuromodulation by electrical stimulation. The second is carrying on-board viral vectors for DNA modification. And the third is modulation by light [optogenetics]’, introducing the truly novel feature of his device. Optogenetics involves using a viral vector, with the replicating properties of a virus but not its pathogenic properties, to introduce DNA coding for a protein type called an opsin into neurons. These opsins are channels controlled by light, which can influence electrical currents in neurons, allowing the modulation of neuronal activity using light without the need for dopamine.

Unfortunately, there are numerous ethical and societal barriers to deploying this technology into mainstream medicine, particularly as viral vectors have not been widely accepted for use in human brains (though they are safe for use in animal and non-human primate models). Nevertheless, Howard says that ‘we are engaged in a discussion with the FDA (Food & Drug Administration) and waiting to hear what the outcome is’, and he seems cautiously optimistic that a version of the KIWI could see its way into clinics soon, ‘within the next year’ he says. Howard thinks that this technology is ‘something that needs to be adapted into the fabric of our society’, emphasising that ‘my goal is to see that things like neurodegeneration are not destroying personal life and personal dignity’.
While the science of decoding the brain is still in its infancy, Howard may have found one language that it uses, perhaps one of many still to be discovered. This language can be used to communicate with the brain to prevent debilitating conditions and significantly improve quality of life even in our twilight years. Technologies such as the KIWI chip are groundbreaking for science and medicine, the next step is for them to push the frontiers of society.
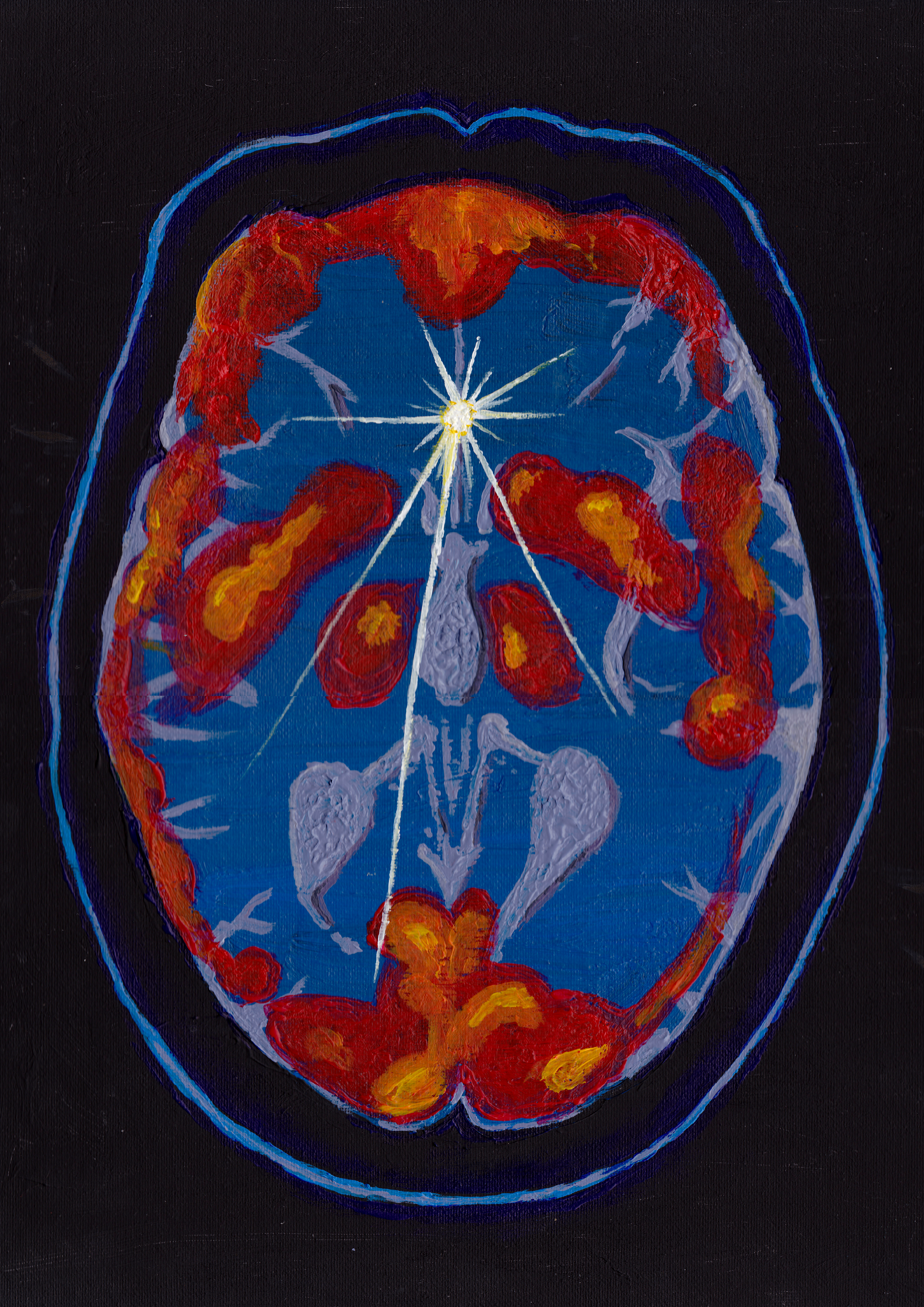
Atreyi Chakrabarty is studying for a PhD in Neuroscience at St Cross College. Artwork by Isabel Caffyn. Cartoon by Ralf Zeigermann.