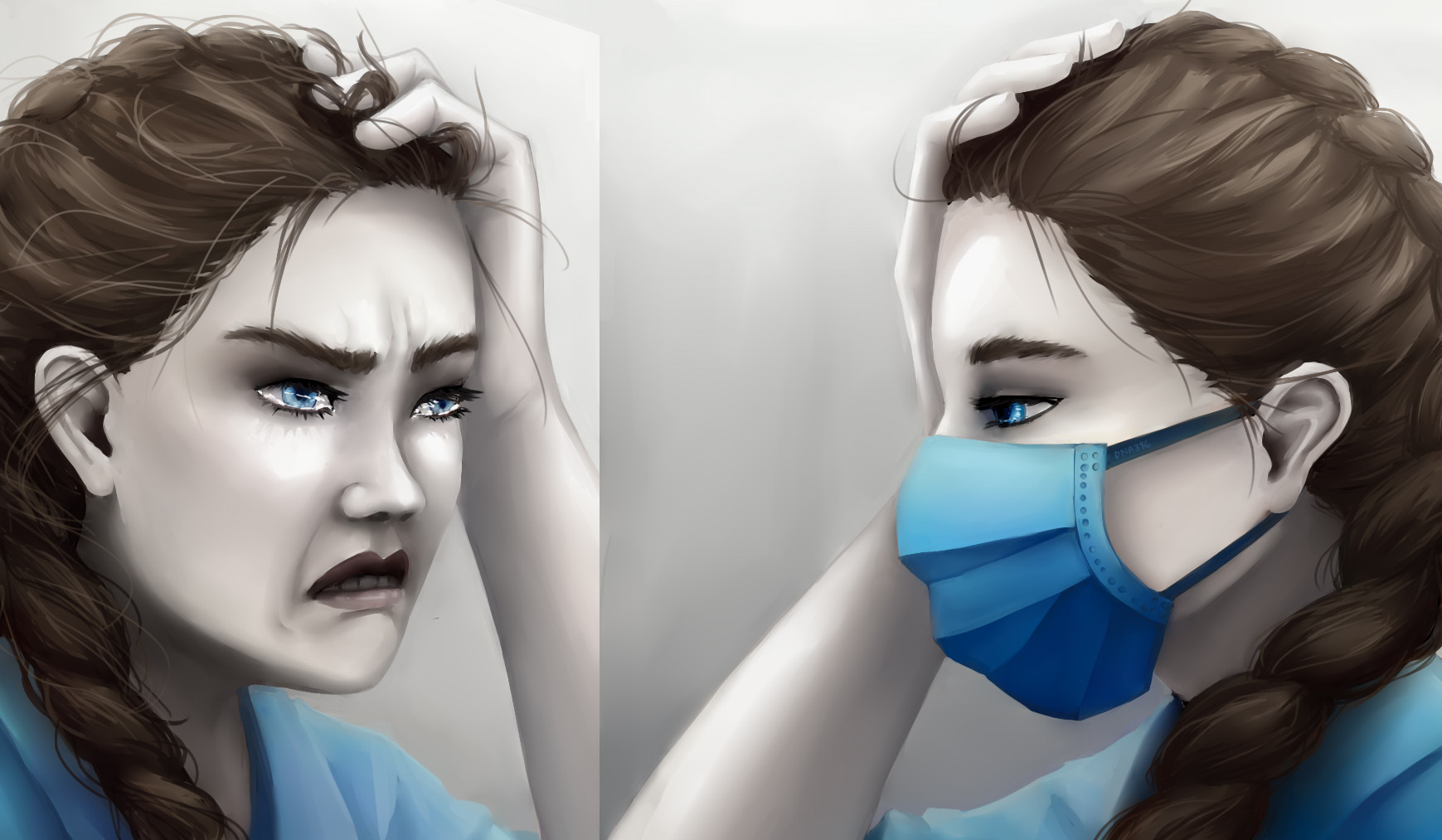
On the frontline of the COVID-19 pandemic, healthcare workers are facing not only a greater risk of infection, but also heightened risk for developing mental health problems. Studies from around the world show that interventions are needed to assist our doctors, nurses, and other healthcare workers as they treat an overwhelming number of highly infectious patients under extraordinary physical and psychological conditions.
Caring for COVID-19 patients is linked with symptoms of depression, anxiety and distress
In a survey involving 34 hospitals in China, a substantial proportion of healthcare workers reported symptoms of depression (50.4%), anxiety (44.6%), insomnia (34.0%), and distress (71.5%)2. Directly diagnosing, treating, and caring for patients with COVID-19 was associated with greater symptom severity. This contact with patients may explain why healthcare workers in Wuhan, a major outbreak centre, and nurses, who tend to have a great deal of direct contact with patients, had significantly worse mental health. Additionally, female healthcare workers reported worse mental health than male healthcare workers. These findings were consistent with findings from another country. In a study of healthcare personnel in Iran, a considerable proportion of healthcare workers also reported symptoms of depression (30.6%), anxiety (28.0%), and distress (20.1%)6. Female healthcare workers were affected more than their male counterparts.
What is causing distress?
Common stressors amongst healthcare workers included feelings of vulnerability, social isolation, and a loss of control, as well as concern about COVID-19’s transmissibility, high morbidity and risk of mortality6. Furthermore, a study in China showed that healthcare workers were affected by feelings of incapability in helping critically ill patients1.
Some of these stressors may be mitigated by psychological interventions. Informed by measures put in place during the SARS outbreak in 2003, one group of researchers recommended the establishment of multidisciplinary mental health support systems, which would be administered by teams involving psychiatrists, psychiatric nurses, clinical psychologists, and other mental health workers. Another recommendation was to screen healthcare workers regularly for depression, anxiety, and suicidality5.
During the pandemic, many mental health interventions were implemented in real time. At a hospital in China, the mental health intervention plan in response to the COVID-19 outbreak included the provision of a psychological intervention medical team, online courses for dealing with common mental health problems, a psychological assistant hotline, and group activities for stress relief1. Meanwhile, a hospital in the US scaled up existing psychiatry services and spiritual guidance, while also offering new services such as self-care resources, virtual support groups facilitated by mental health providers, individual counselling, and 24/7 crisis management3.
Psychological support isn’t the only solution
Several concerns were shared by healthcare workers across multiple countries. Studies from Iran, China, and the US demonstrated that healthcare workers were especially troubled by a lack of personal protective equipment1,4,6, a lack of testing, which led to workers to worry whether they had unknowingly contracted the disease4,6, and personal health and the health of family members1,2.

Other stressors were specific to healthcare workers in each country. For healthcare workers in the US, key concerns included personal and family needs like childcare, housing, transportation, and food. Additionally, they worried about their capacity to provide appropriate medical care if deployed to a new area, as well as about their access to accurate and up-to-date information4. Meanwhile, healthcare workers in China were troubled by how to deal with patients refusing to quarantine at the hospital or otherwise cooperate with medical measures as well as the difficulty of resting without interruption1.
Several practical interventions were adopted in response to these needs. At a hospital in the US, the response plan for maintaining the emotional wellbeing of healthcare workers included the provision of transit options and alternative childcare arrangements, rest areas and temporary accommodations, and in-house meals3. The hospital also enhanced communications to deliver current, reliable, and reassuring information comprised of a daily newsletter with links to a comprehensive website, a weekly system-wide town hall meeting, and wellness messages from mental health experts3. At a hospital in China, the practical response plan for protecting the mental health of overworked healthcare staff included a rest area, leisure and relaxation exercises, and counsellors who visited the rest area to discuss work challenges1.

We must protect our healthcare workers
Directly managing patients affected by COVID-19 was associated with symptoms of depression, anxiety, insomnia, and distress in healthcare workers. Common psychological sources of distress included feelings of vulnerability and worry about COVID-19’s transmissibility, morbidity, and mortality. These concerns were addressed by providing psychological resources, like a 24/7 crisis response, online courses and virtual support groups, and scaling up counselling services. However, distress was also attributed to practical needs, such as a lack of personal protective equipment, testing for healthcare workers, and concerns about the wellbeing of family members. These practical challenges were tackled by creating a rest area staffed by counsellors, offering childcare and temporary accommodation, and by providing up-to-date, reliable communications from hospital administration.
Healthcare workers are undoubtedly facing a number of stressors unique to the current pandemic, which may erode their mental wellbeing and resilience. It is critical for institutions to support the mental health of their staff members and provide access to much-needed resources, so that healthcare workers may carry on with their critical work of caring for patients.
Sources & further reading
[1] Chen Q, Liang M, Li Y, Guo J, Fei D, … Zhang Z (2020). Mental health care for medical staff in China during the COVID-19 outbreak. Lancet Psychiatry, 7.4: 14-16.
[2] Lai J, Ma, Wang Y, Cai Z, Hu J, … Hu S (2020). Factors Associated With Mental Health Outcomes Among Health Care Workers Exposed to Coronavirus Disease 2019. Journal of American Medical Association, 3.3: 203976.
[3] Ripp J, Peccoralo L, Charney D (2020). Attending to the Emotional Well-Being of the Health Care Workforce in a New York City Health System During the COVID-19 Pandemic. Academic Medicine, In Press.
[4] Shanafelt T, Ripp J, Trockel M (2020). Understanding and Addressing Sources of Anxiety Among Health Care Professionals During the COVID-19 Pandemic. Journal of American Medical Association.
[5] Xiang Y, Yang Y, Li W, Zhang L, Zhang Q, … Ng CH (2020). Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry, 7.3: 228-229.
[6] Zhang SX, Liu J, Afshar Jahanshahi A, Nawaser K, Yousefi A, … Sun S (2020). At the height of the storm: Healthcare staff’s health conditions and job satisfaction and their associated predictors during the epidemic peak of COVID-19. Brain, Behavior, and Immunity.
Title image by Tiffany Duneau.