Sophie Thompson
The digitisation of healthcare is not a new idea—indeed it was a clear ambition of the NHS Long Term Plan, published in January 2019, which proposed that all patients should have the right to a ‘digital first’ primary care offer by 2023/2024. The pandemic, however, necessitated a much more rapid realisation of this vision to protect both patients and doctors, and GP surgeries across the country have found themselves having to move to remote methods of consultation and online triaging in a very short space of time. In essence, the pandemic prompted something of a ‘telehealth revolution’—but will progress continue once things get back to normal?
The first big change that many people will experience when booking an appointment with their GP is a digital triaging system, asking them to give an account of their concerns and history through a series of tick boxes and free text boxes. This then goes straight to the doctor, who decides how urgently the patient needs to be seen. Whilst this may seem a little impersonal and cumbersome, particularly when you can’t decide which category on the list your problem falls under and which box to tick, it has clear benefits whether COVID-19 is a factor or not. For one, doctors can triage their own patients and decide who needs to be seen to first, which takes the responsibility away from reception and admin staff with less clinical knowledge. Moreover, although access concerns have been raised about those who aren’t so tech savvy, receptionists have said that giving patients the option of online consultation actually frees up the phone lines and gives them more time to talk to those who cannot or do not want to use the digital system. One online system which the NHS has fast tracked into a huge number of GP surgeries is eConsult, accessible via the NHS app. By the 30th April 2020 this was available to over 2200 GP practices nationwide, covering 20 million patients.
The second key feature of the telehealth rollout is the ability to deliver consultations remotely, which includes telephone consultations but also video calls and even an SMS message if a query only requires a quick answer. This clearly has advantages in the pandemic, reducing viral transmission and protecting both doctors and patients, as well as allowing doctors who are self isolating to continue working from home. However, for the busy shift worker and the housebound elderly gentleman alike, it surely has potential looking ahead to the future too. It saves both time and travel, and means that a simple medication query that would’ve previously taken a ten minute appointment slot can be answered in a matter of seconds over a text.
That being said, can a remote consultation provide the same quality of care as a face to face consultation? Doctors are taught from medical school that body language and non-verbal cues are just as important as what a patient tells you. Little things as simple as how they sit down can all give essential diagnostic cues. There is also the fact that, as we all know from trying to stay in touch with friends spread around the country, a FaceTime just isn’t as personable as a face to face meeting. This is crucial as a patient feeling at ease and connected to their doctor can make the difference between them disclosing vital information and keeping it to themselves.
So what’s the verdict? Whilst there is undoubtedly a need to take a breath once the pandemic is over and review the situation, it is hard to see GPs ever returning to how they were. I can’t see doctors being replaced by robots any time soon, and rightly so, but we must embrace change and acknowledge that telehealth has a valuable role to play in the future of General Practice.
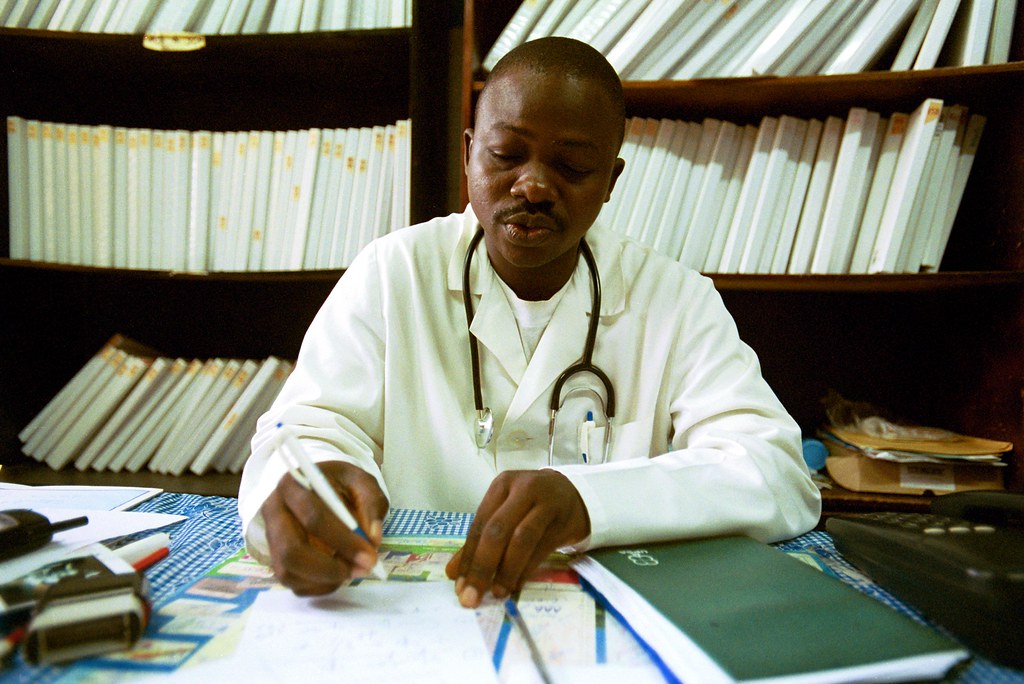
Image credit: “A doctor looks over a patients medical records” by World Bank Photo Collection is licensed under CC BY-NC-ND 2.0