by Tamilore Awosile, Year 13, The Haberdashers’ Aske’s Boys’ School, Hertfordshire.
I was born with sickle cell anaemia, a genetically inherited blood disorder which affects approximately 4.4 million people worldwide. In the UK, it is particularly prevalent in people of African or Caribbean heritage.
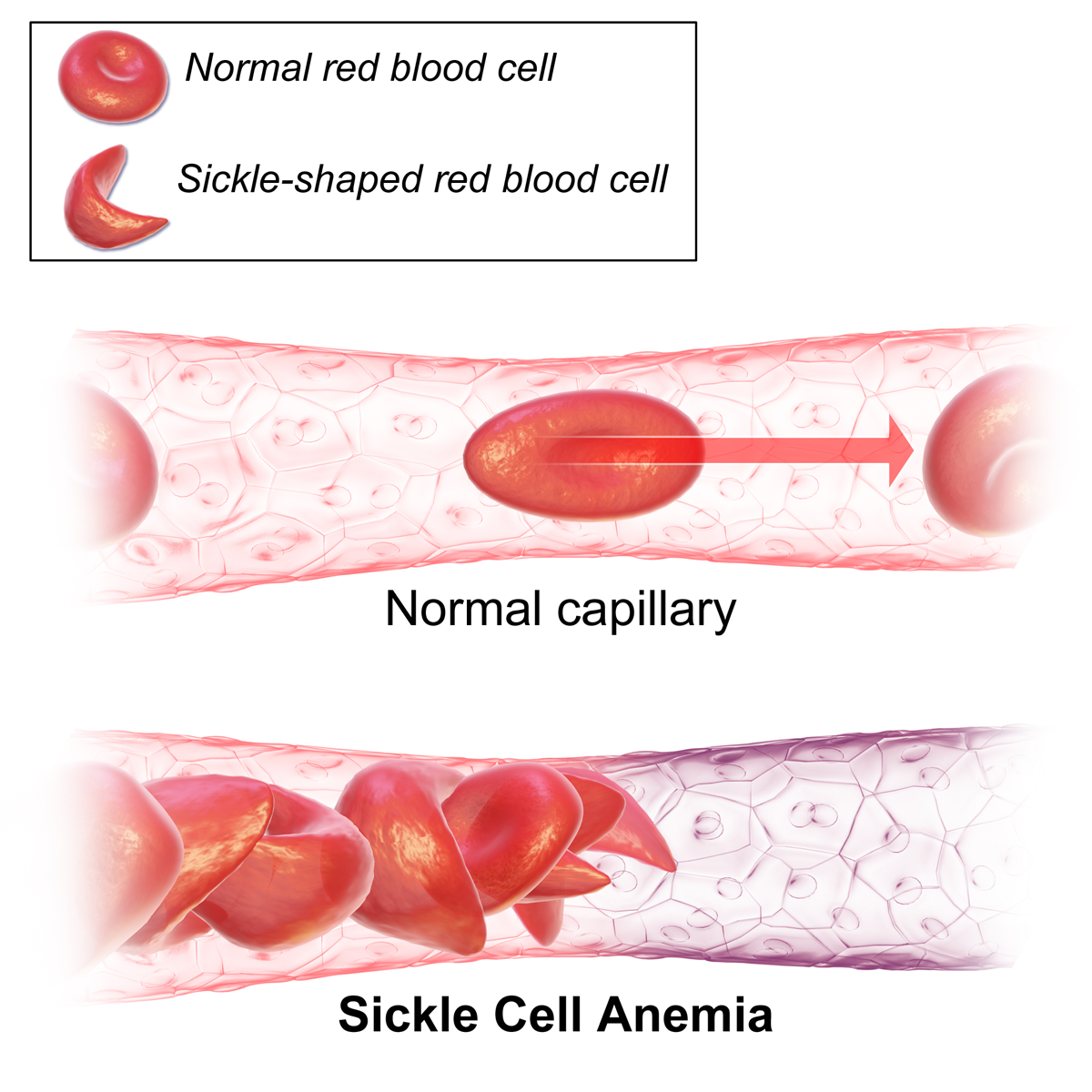
Sickle cell is caused by a mutation in the DNA of the HBB gene responsible for producing the beta-globin chains in haemoglobin, the oxygen-carrying molecule in red blood cells. The mutation causes deoxygenated haemoglobin molecules to stick together inside red blood cells, producing abnormal, sickle-shaped red blood cells.
Normal red blood cells are round, allowing them to flow easily through blood vessels. However, due to their shape, sickle blood cells can become stuck in blood vessels, causing a painful episode known as a “crisis”, which can be severe and cause debilitating pain. Other problems associated with this condition include an increased risk of serious infections and anaemia, as well as more severe complications such as acute chest syndrome and stroke. Sickle cell is inherited when both parents are carriers of the allele for the mutated HBB gene. In this scenario, there is a 1 in 4 chance of having a child with sickle cell. I am that 1 in 4 chance.
At nine, I was diagnosed with right hip avascular necrosis, a complication caused by my sickle cell. It occurs when sickle cells block the blood flow in the vessels which supply the hip bone. Consequently, the bone tissue does not get enough oxygen and dies. The loss of tissue caused my right femoral head to change shape, and it is now one centimetre shorter than my left hip. This means I walk with an often-pronounced limp, which is managed by wearing an orthotic shoe lift. Personally, this has been one of the most challenging aspects of living with sickle cell, both emotionally and physically. It has limited my ability to participate in contact sports, meant I’ve had to use a crutch for extended periods of time, and has made me self-conscious about the way I walk. Unlike other aspects of living with sickle cell, which are very much hidden, my avascular necrosis is very much out on display.
On my fifth birthday, I experienced my most severe complication with sickle cell: acute chest syndrome. I was on the verge of respiratory failure, with dangerously low levels of blood oxygen when I was intubated, rushed to intensive care, and put on a ventilator. It was in the aftermath of this incidence that I was first prescribed hydroxycarbamide. Hydroxycarbamide is the only medication licensed in the UK for the prevention of recurrent painful crises and acute chest syndrome in patients with sickle cell. Around 13% of patients with sickle cell anaemia with the UK National Haemoglobinopathy Registry use hydroxycarbamide. Hydroxycarbamide works by increasing fetal haemoglobin levels in red blood cells, preventing them from turning into sickle cells, thereby reducing episodes of painful crises. Hydroxycarbamide has completely revolutionised my quality of life. It has led to a reduction in painful crises, incidences of acute chest syndrome and hospital admissions. This has allowed me to focus on leading a normal childhood and adolescence.
Science has the potential to further impact the lives of sickle cell patients. However, this has been inhibited by many socioeconomic factors, something reflected in the resources currently allocated to sickle cell research. In the US, sickle cell (a condition mainly affecting ethnic minorities) affects three times more people than cystic fibrosis (a condition which primarily affects the Caucasian population). However, cystic fibrosis receives 3.5 times more funding from the National Institutes of Health, and 400 times more funding from national foundations. With a fairer allocation of resources, there is so much more science can achieve for patients with sickle cell, helping to transform their everyday lives.
Science has improved people’s lives throughout history and will continue to do so. My life is a prime example of this. The hydroxycarbamide I take daily, the ventilators that breathed for me in intensive care, and the transfusion machines that have exchanged my blood only exist because someone dedicated countless hours to research. In the future, I hope to pursue a career in scientific research. I want to be part of life-changing discoveries.