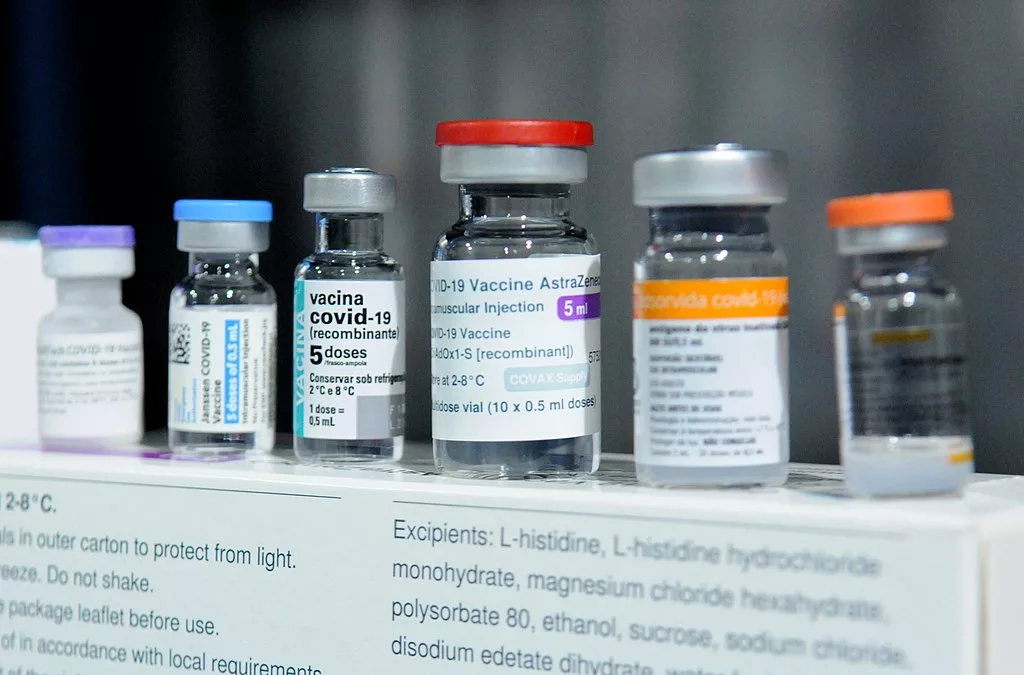
An array of vaccines developed against COVID-19. Agência Brasília, CC BY 2.0, via Wikimedia Commons
As we near the three-year anniversary of worldwide lockdowns, social distancing, and the global wrath of COVID-19, it’s fitting that we reflect on the years that have passed. I once heard a talk where someone said that the more effective our public health measures are, the more people will say we went too far with our pandemic restrictions. While it may be true that our triumphs have been concealed by complaints and frustration, our mistakes have stuck out like a sore thumb.
Let’s start from the beginning. On March 11th, 2020, the World Health Organisation (WHO) declared the novel coronavirus strain a pandemic. It didn’t take long after this for the world to recognise the seriousness of COVID-19, and for global vaccine efforts to emerge. Less than a year from the worldwide shutdown, vaccines were in the arms of individuals around the globe.
Previous years of mRNA vaccine research certainly played a role in the speed with which we developed a functional vaccine against the virus, but that should not undermine what an achievement this was. In fact, many believed that a functional vaccine would take over a year and a half to reach fruition. Even a single dose of a Pfizer-BioNTech or AstraZeneca COVID-19 vaccine was associated with a decrease in household transmission by 40-50%, while significant reductions in severe disease and hospitalisation were also attributable to vaccination. The success of the vaccine and initial global efforts toward curbing COVID-19 spread should be celebrated, as they certainly played a significant role in reducing the spread and morbidity associated with the disease.
Although countries all around the world, including the United Kingdom, United States, Germany, China, Taiwan, and more, focused many of their resources on producing a vaccine, the same cannot be said about its distribution. Originally, countries took a “me first” approach to their vaccine rollout, allocating their vaccination stocks to nationals. It felt like each country was riding on an aeroplane: securing their own oxygen mask before helping others.
The issue is that, as vaccination production ramped up, and as more and more jabs were administered, the focus never really shifted to global vaccine equity. In March 2022, two years after the start of the pandemic, 74% of people in high-income countries had received at least one COVID-19 vaccination, compared to only 14% in low-income countries. Tackling issues such as cost, transport, and accessibility, which contributed to these staggeringly low vaccination rates, was not made a priority for many high-income countries.
A clear example of a lack of commitment to global vaccine equity was seen in the dissemination of booster shots. While many countries still lacked access to initial doses of the vaccine, many wealthy countries were administering booster shots: additional jabs to those who had already received a primary vaccination series. In August 2021, the WHO called for a pause on booster shots in healthy adults in an attempt to address the issue of global vaccine inequity. However, many countries chose to ignore the call to action and continued to move forward with booster doses at the time.
There were, however, international efforts to address vaccine inequity. Most notably, COVID-19 Vaccines Global Access (COVAX) was a global initiative developed in April of 2020 to ensure equitable access to COVID-19 vaccine technologies. Despite its best efforts, many of the ambitious COVAX vaccination goals were not met throughout the pandemic. COVAX was meant to operate in two fashions: first, by working with COVID-19 research and development, negotiating fair prices for countries, and ensuring equal vaccine access to all participating countries upon development of a vaccine; and second, by receiving donations from organisations and countries to procure vaccines for lower-income countries.
Initially, countries including the United States and China opted out of COVAX, choosing to focus their energy on national vaccination efforts. Funding for COVAX became an issue, and so did vaccine procurement, as many countries made significant deals on their own to receive vaccine supplies. Although COVAX had great intentions to ensure equitable vaccine access, a lack of meaningful participation from wealthy countries stunted the initiative’s success.
Not only are there severe implications for individuals in these unequally vaccinated countries, but there are also global consequences of uneven vaccine distribution. Many of the novel COVID-19 variants that spread during the numerous waves of the pandemic were born out of countries with very low vaccination rates. Low rates of vaccination result in higher levels of transmission. With increased person-to-person spread, there is also a greater risk of the virus mutating into novel strains. The lack of focus on vaccine equity was not only a global letdown to individuals in lower income countries to ensure their safety amid the wrath of COVID-19, but it also reflected a failure to understand the global benefits of equal vaccine distribution.
In countries where vaccines were available, vaccine hesitancy was a plaguing issue. All around the world, people were sceptical of novel vaccine technologies, worried about reported vaccine side effects, and suspicious of the accelerated rollout of COVID-19 vaccines. Consequently, many were hesitant to get the jab. In response, many countries enforced vaccine mandates. Mandates varied based on country. Some countries, including the Czech Republic and Greece, mandated that older or at-risk individuals get the jab, while in others, people of certain professions like federal workers in the United States and Canada, were required to receive the vaccine. In certain countries like Austria, every eligible adult was required. Among countries that opted out of vaccine mandates, some decided to impose restrictions on those who were unvaccinated, such as restricting access to public spaces.
Although high levels of vaccination were necessary to curb transmission, take the strain off healthcare systems, and reduce the risk of novel variants, the approaches that were taken were not necessarily the most effective, nor the most inclusive. Many of those who were hesitant and/or unwilling to take the vaccine were those belonging to racial and ethnic minority groups. While the rapid pace at which the vaccine was developed contributed to a lot of hesitancy, so too did the marginalisation experienced by these groups.
There has been a history of the systemic oppression of racial and ethnic minority groups at the hands of government and healthcare institutions in our society. Take, for example, the Tuskegee Syphilis Experiment in the United States, where African American men were denied effective treatments for syphilis for years. Or in Canada, where Indigenous children were stripped from their families, at the hands of the Canadian government, and forced to attend residential schools with appalling conditions.
You need not look any further for examples of these injustices than here in the UK where racial health inequalities are rampant. These are just a few examples of detrimental actions by government and healthcare institutions that have negatively impacted minority groups. These examples, coupled with our knowledge of widespread racial health disparities, highlight how governments and healthcare systems have let down racial minority groups on many occasions, fuelling a sense of mistrust within these communities.
Early in the pandemic, these same government and healthcare institutions were asking, and sometimes mandating, that these communities roll up their sleeves to receive a novel vaccine. Despite the hesitancy caused by the rapid push-through of the vaccine programme, the systemic oppression and marginalisation of minority groups resulted in elevated levels of hesitation and mistrust among such communities. Of course, there were others who were opposed to the vaccine and carried their own hesitations, but we must understand that many of those who were vaccine-hesitant were already marginalised individuals feeling disproportionately affected by measures encapsulating compulsory vaccinations or restrictions based on vaccination status. Sure, widespread vaccination was a necessity of public health strategies, but hopefully when the next pandemic occurs we can employ strategies that do not exacerbate long-standing societal inequalities and do not perpetuate mistrust in these institutions.
It should come as no surprise that the pandemic resulted in serious social and political divides. While the early days of the pandemic were fuelled by support for the collective good and the need to protect the most vulnerable, it quickly transpired that these widespread views would not last for long. As people started to realise that a two-month lockdown would not halt the pandemic, nor would widespread vaccinations, a schism between those who believed it was time to move on with regular life, and others who felt strongly that measures should remain in place to protect the health and wellbeing of everyone emerged.
A line was quickly drawn in the sand: there were those who were vaccinated versus those who were not, and those who supported widespread public health measures versus those who wanted life to return to normal. The pandemic was a breeding ground for social divide. Through this, productive conversation and healthy debate fell to the wayside. Much of this divide was fuelled by misinformation on both sides, selective bias in only seeking out information that supported one’s own point of view, and in many cases, a complete lack of empathy for those who had different opinions.
I’ll admit, I was guilty of the same. As a medical student and the daughter of someone who is immunocompromised, I felt my blood boil when I heard people take such offence to wearing a mask. There were days when scrolling through Twitter and seeing one person or another complain about public health measures would drive me up the wall. There were also days when I felt like I had to be unwavering in my stance, to be more radical than the other side, just to get my point across. But I realised that, in doing so, I was part of the problem.
What I’ve come to realise is that the downfall in our pandemic response, which is still our downfall to this day, was a lack of empathy, understanding, and collaboration towards most, if not all, of the issues we faced. We went through, and are still going through, a global pandemic. The word ‘global’ implies that there would likely be a unified and collective response—but there wasn’t. If there had been, then we wouldn’t have countries who are still not vaccinated. We wouldn’t enforce measures without considering how they would exacerbate inequalities. We wouldn’t be shouting at people who disagreed with us. The world went through a global pandemic, but much of the world had a very individualistic response.
I’m not an epidemiologist or an infectious diseases expert by any means—I have no idea when the next pandemic will be or what it will look like. I don’t even know when this one will be over. But what I do know is that what we lacked in this pandemic response was working together, respecting the complexities of different lived experiences, and listening. Global issues can’t be solved with individual-level solutions. National policies can’t be implemented without considering the impacts of all those affected. Compromise can’t be reached unless people dedicate themselves to hearing each other out. I hope that we acknowledge these lessons and take what we have learned, not only into the next pandemic, but in every global issue we face in the future.