Recent evidence supports the use of fosravuconazole in treating the flesh-eating disease, Mycetoma. However, external factors means treatment is not that simple. Photo credit: Photo by Towfiqu barbhuiya on Unsplash
Mycetoma, a chronic, progressively destructive disease, has long been one of the most neglected infections. Often referred to as a “flesh-eating” disease, current treatments are expensive, ineffective, and often accompanied by a multitude of side effects. Recent results from a first-of-its-kind trial have presented hope for a new treatment for this infection, in the form of a simple over-the-counter medicine.
Often referred to as a “flesh-eating” disease, current treatments are expensive, ineffective, and often accompanied by a multitude of side effects.
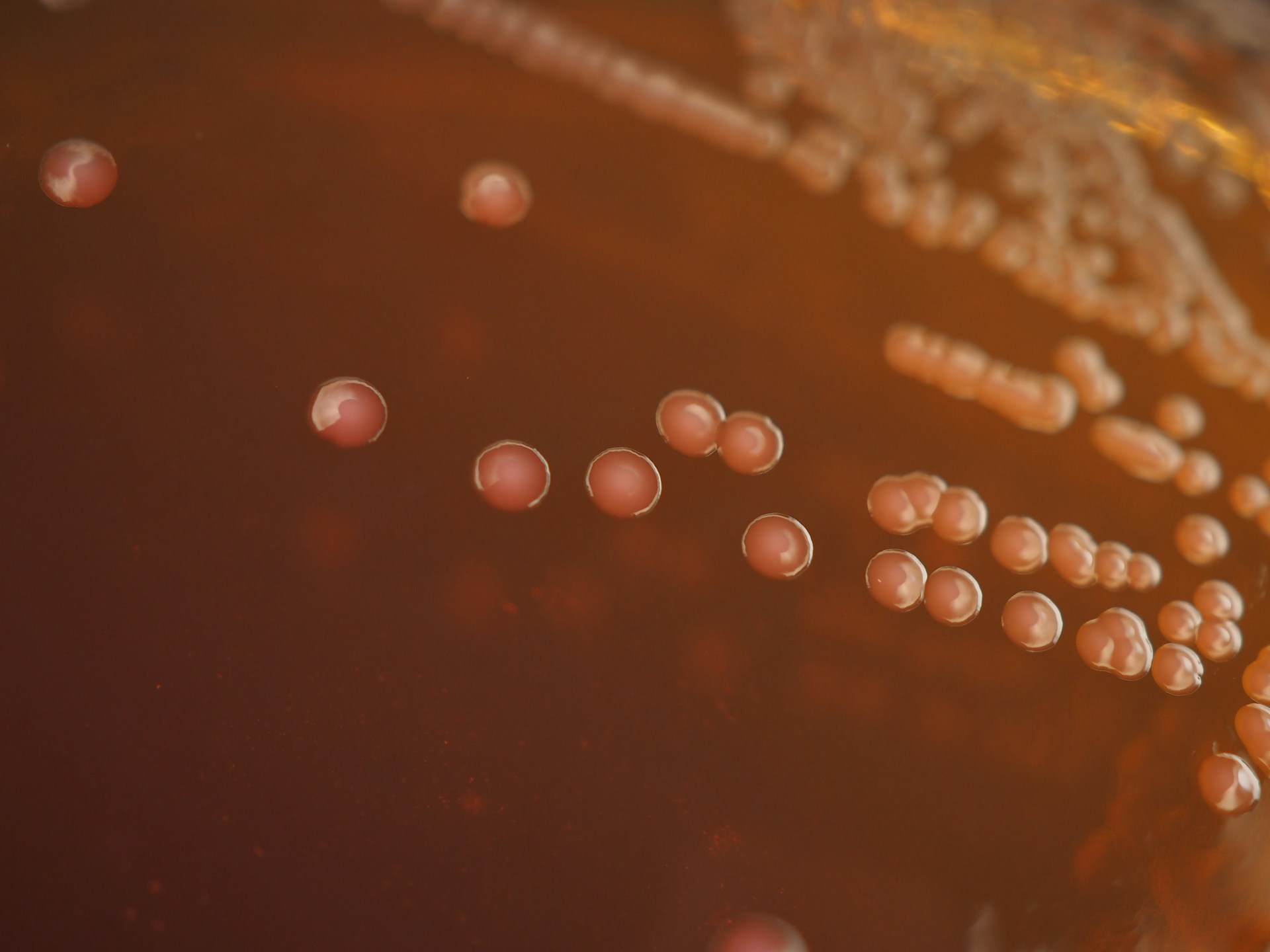
Mycetoma is a disease which may not be in the public consciousness in the same way as more acute and dramatically-presenting infections, such as scabies, but it could certainly benefit from more attention. Caused by injury as simple as a thorn-prick, the disease is most commonly fungal in origin and affects skin, muscle, and bone. Tissue is progressively destroyed throughout the infection, and often amputation is required to prevent further spread.
Current treatments have an abysmal efficacy rate in the field of approximately 25-35%, and whilst the prevalence of mycetoma is known to be common at specific latitudes—including Sudan and Mexico—the overall global impact of the disease is unknown. In 2016, the World Health Organisation (WHO) placed it on its list of 20 neglected tropical diseases. Despite major drug development companies largely ignoring this devastating disease, a coordination of efforts has championed a world-first double-blind clinical trial for a new treatment regimen.
In 2016, the World Health Organisation (WHO) placed it [Mycetoma] on its list of 20 neglected tropical diseases.
Mycetoma is especially common in young adults, with people of low socioeconomic backgrounds most severely affected. Infection may initially appear as a firm mass under the skin, often on the foot, which increases in size over time and forms sores. While a bacterial infection may be treated with antibiotics, for fungal mycetoma there are severely limited effective treatments available. As a chronic disease, meaning it persists over time, certain social stigmas can negatively impact mental health. The extensive and often inaccessible treatment plan required for current therapies, combined with the impact of limb loss on livelihood and childhood freedoms, means that more effective protocols are necessary.
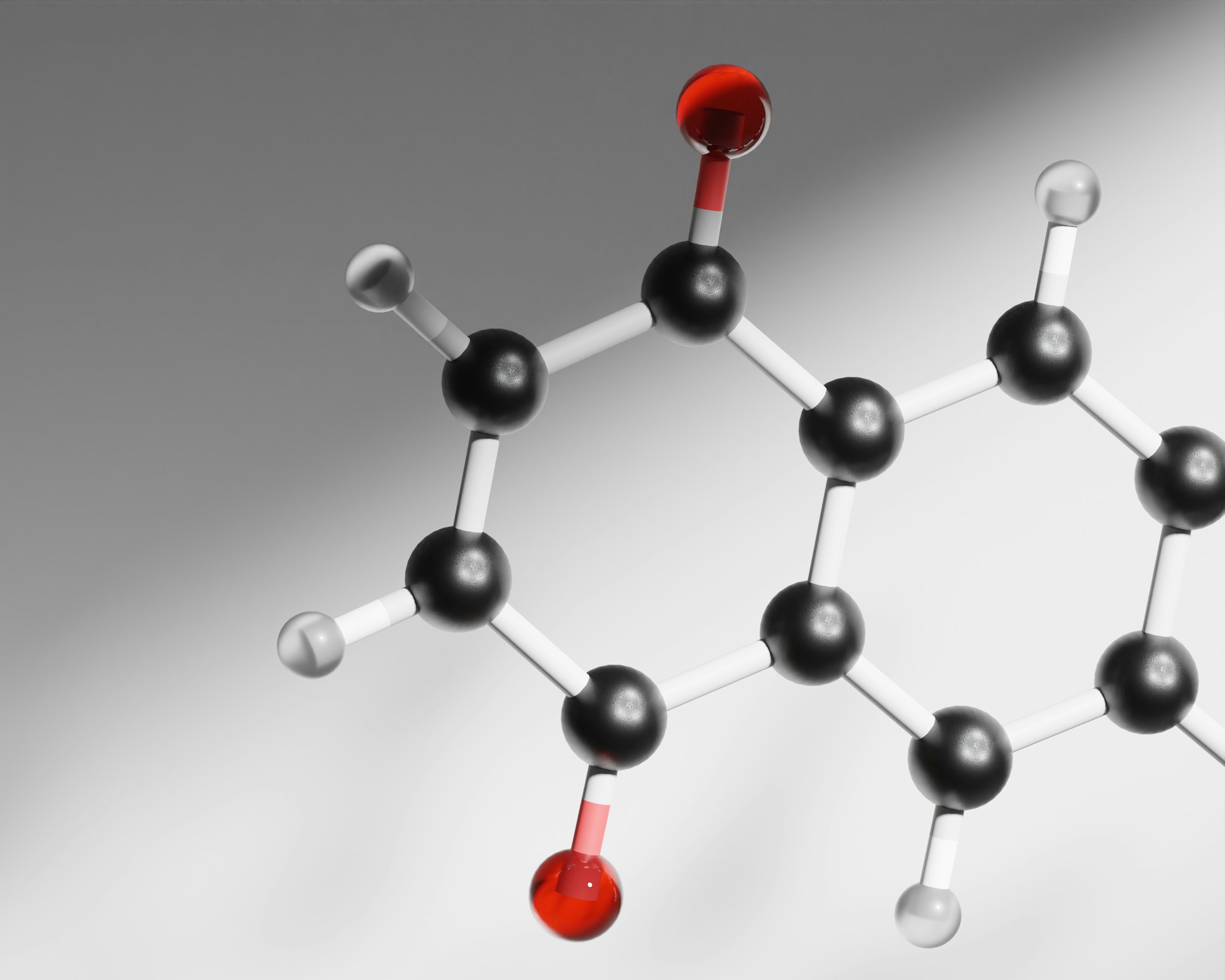
In 2017, the Drugs for Neglected Diseases Initiative (DNDi) partnered with the Mycetoma Research Centre (MRC) in Khartoum, Sudan, and the pharmaceutical company Eisai Co. Ltd of Japan to enlist patients in the first clinical trial for a new treatment. This trial compared the efficacy (how well the drug works) of a common nail fungal treatment fosravuconazole with the current first-line treatment for mycetoma (itraconazole). As a double-blind trial, neither the experimenters nor patients knew which drug they were receiving. Itraconazole, while up to 80% effective if the full course of medication can be taken, is inaccessible to many suffering from the disease and has to be taken four times a day with food for up to a year. Meanwhile, fosravuconazole can be administered weekly and is effective even at low doses; this gives the drug a clear advantage in fungal cases.
Preliminary results of this trial, from the Phase II stage—meaning efficacy is being tested on groups of human subjects numbering in the 100s—were presented at the 13th European Congress on Tropical Medicine and International Health (ECTMIH) in Utrecht, Netherlands, in late 2023. Fosravuconazole, the new drug, was shown to have an efficacy rate of 85% at 200mg and 65% at 300mg doses respectively, a higher-than-expected finding. The comparable efficacy to itraconazole indicates fosravuconazole as a preferable treatment, given the greater convenience of this medicine.
Another important aspect of the drug is a lack of interaction with other medications, a feature particularly important in areas where diseases such as tuberculosis or HIV are common. Professor Ahmed Fahal, Professor of Surgery at the University of Khartoum, and MRC Director, states, “This reduces the pill burden for patients significantly, with only eight tablets per month versus the current 120. This will greatly improve adherence and convenience for patients”.
In recognition of the public health impact of mycetoma, the limited epidemiological data, and the lack of disease surveillance, the Sudanese Ministry of Health has given the green light for fosravuconazole treatment under controlled conditions. However, with the outbreak of conflict in April 2023, the breakthrough in treating the fungal disease may be trickier to implement than expected. As the only WHO Collaborating Centre for mycetoma and neglected tropical diseases, the MRC has had to close its doors. Normal treatment protocols and the ability to access free care have been disrupted.
Ahmed Fahal writes eloquently in the Royal Society of Tropical Medicine and Hygiene in mid-November of laboratories “silent and idle”, “inaccessible or compromised”, and “the seamless synergy between research, diagnosis, and treatment…threatened”. Initiatives to deliver entrepreneurship and skills training to those affected by mycetoma have been halted. He calls upon the international health community to rally around a group of scientists working tirelessly to fight for the treatment of a disease for so long neglected—receiving that support sooner rather than later could be invaluable.