New studies have revealed that mpox has been transmitted human-to-human for years before once thought. Image credit: Claudio Schwarz via Unsplash.
According to new research, mpox (formerly called monkeypox) had circulated in humans for several years prior to the 2022 global outbreak. By analysing genetic mutations between earlier viral samples and those from 2022, researchers inferred that human-to-human transmission had been in place since at least 2016, reshaping our former view of this virus’ predominantly animal-to-human transmission.
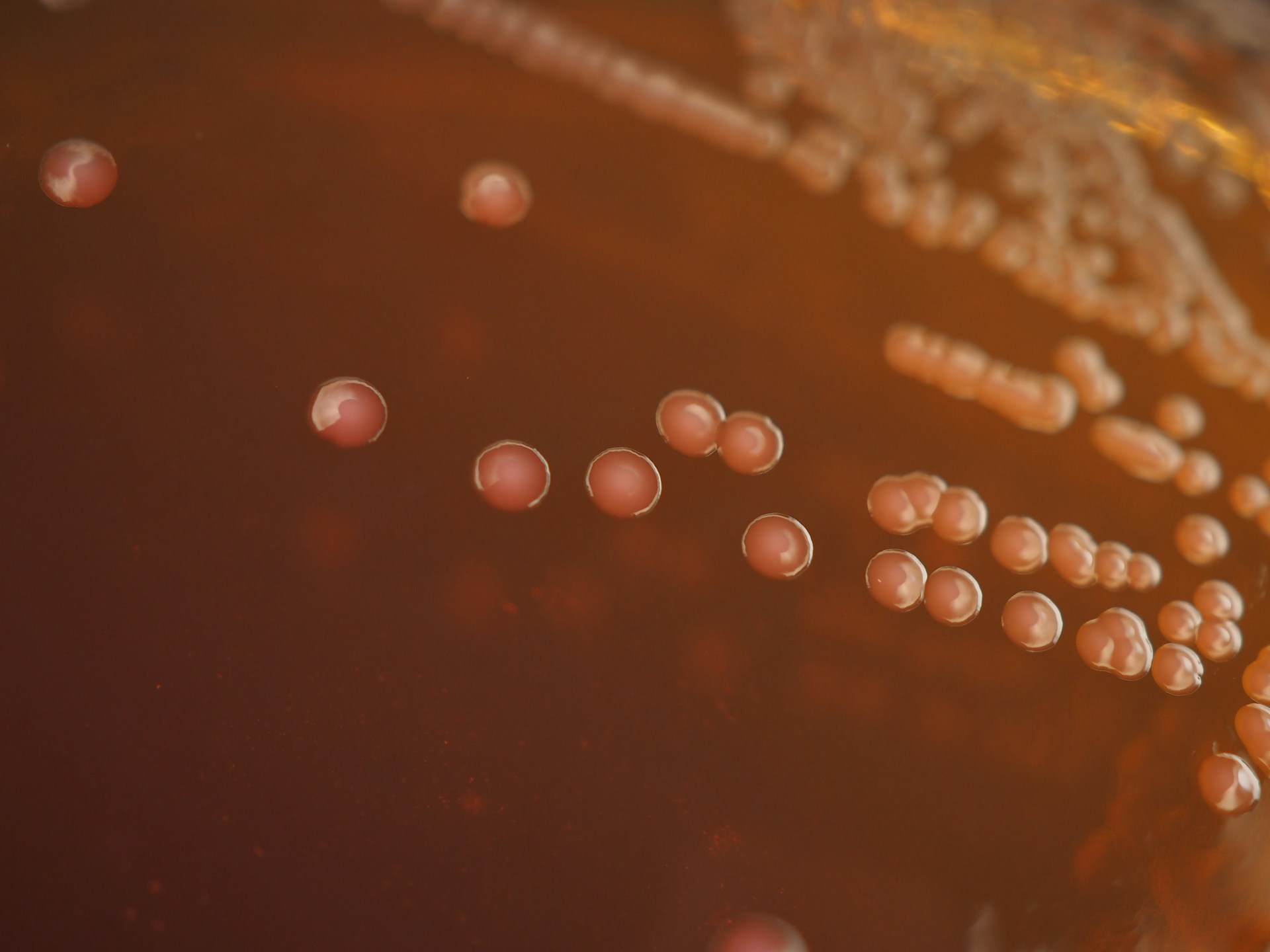
Mpox is a disease caused by the virus MPXV. Though common symptoms consist of skin rashes and fevers, it can also cause serious illness and lead to death in humans. Following its discovery in 1958 in captive monkeys, there have been cases of mpox in humans since the 1970s, predominantly in West and Central Africa where there are rodent hosts for the virus. Therefore, this disease has classically been seen as zoonotic (spreading from non-human animals to humans) with occasional spillovers and transmission in humans.
The 2022 outbreak of mpox caused international concern as it was the first time that a significant spread of cases to countries beyond those with known animal reservoirs for the virus occurred, leading to an all-time peak in the number of cases. According to the CDC, cases were reported across 116 countries, of which only seven had mpox cases historically. Although the mortality rate of the mpox variant responsible for this outbreak is likely below 1%, with it causing at least 166 deaths (from 1st January 2022 up to 21st November 2023), it is much higher for those with compromised immunity. Transmission occurred predominantly between men who identified as having sex with men, leading to stigmatisation and misinformation. Scientists at the time warned that this stigmatisation could impact public health, as global responses to the mpox outbreak were hindered by political leaders who had hostile attitudes towards the LGBTQI+ community and their healthcare rights. Therefore, understanding this outbreak can both help with destigmatisation as well as potentially inform effective policy interventions to prevent further illness and mortality.
The 2022 outbreak of mpox caused international concern as it was the first time that a significant spread of cases to countries beyond those with known animal reservoirs for the virus occurred, leading to an all-time peak in the number of cases.
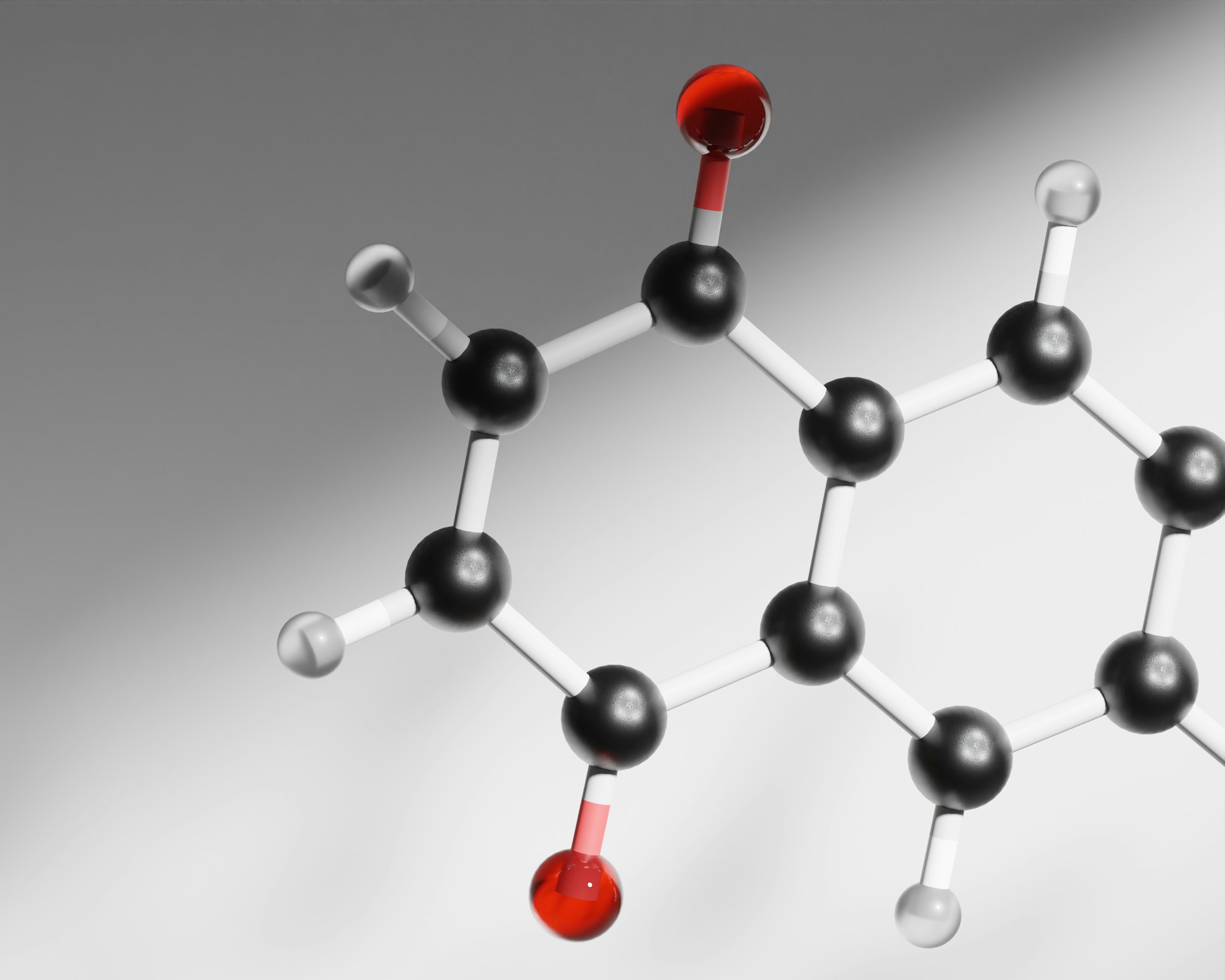
To understand this outbreak, authors of the new study compared viral genomes from the 2022 outbreak with samples from infected humans in 2018 and found that there had been far more mutations than expected. Based on an outbreak in chimpanzees Pan troglodytes, MPXV has an expected mutation rate of one nucleotide change every three years (i.e. a change in one “letter” of the genetic code). Surprisingly, researchers identified 42 differences between the 2018 and 2022 samples. Whilst these mutations could be down to the virus adapting to infect humans in 2022, the high rate and nature of the mutations suggests otherwise. MPXV’s DNA genome contains 200,000 bases (A, T, G or C), which code for the proteins that allow the virus to survive and reproduce. Most mutations involved a change in the genetic code from TC to TT or GA to AA: a signature of the APOBEC3 enzyme. APOBEC3 is an anti-viral enzyme in the human immune system that attacks viral DNA when exposed to viruses.
These mutations seemed to be a genetic footprint of the human immune system interacting with this virus. Due to the high number of mutations, it is likely that these changes occurred through sustained transmission between humans rather than repeated infections between animals and humans.
The B.1 lineage which primarily caused the 2022 mpox outbreak belongs to a larger clade (evolutionary group sharing a common ancestor) of mpox viruses: clade IIb. Sequencing samples from previous years in this clade allowed researchers to extrapolate back in time to estimate when these characteristic mutations first appeared in ancestors of B.1. Accounting for some uncertainty, the researchers dated the first mutations—and therefore start of human circulation—as 2016 at the latest.
Accounting for some uncertainty, the researchers dated the first mutations—and therefore start of human circulation—as 2016 at the latest.
Long-term, this attack by the human immune system could weaken the virus if harmful mutations accumulate over time, hindering its ability to infect. However, how long this would take and how this would balance with opposing evolutionary forces restoring MPXV’s ability to infect remain unknown.
These results coincided with another recent study which reported the circulation of a different lineage of mpox (A.2) in Nigeria prior to 2022. Although this study was more restricted in its sampling and findings, the authors also found signals of APOBEC3-induced mutations, corroborating these conclusions based on genetic impressions of human-mpox interaction.
This revelation of sustained human transmission for many years prior to the 2022 outbreak goes against the traditional view of mpox as a predominantly zoonotic disease. Mpox cases continue to circulate globally, albeit at relatively low levels, highlighting the need for global surveying to understand human-to-human transmission of this virus. Furthermore, this pre-outbreak circulation could have laid the foundations for the outbreak by giving the virus increased opportunity to evolve and become more infectious in humans. Therefore, ongoing sampling of virus genomes from around the world could help epidemiologists predict and understand future outbreaks, both for mpox and its successors.