Will the current bird flu outbreak turn into another pandemic? Photo credit: Fusion Medical Animation via Unsplash
Recent news of the first bird flu-related human death in the US, following the virus’s unexpected spillover into cattle last year, has raised serious concerns about global pandemic preparedness. These worries are reminiscent of the unresolved gaps in preparedness before the COVID-19 pandemic. With expert opinion divided regarding the immediate threat level, the question remains: How worried should we be?
What is H5N1 and why does it matter?
H5N1 is a highly pathogenic avian influenza subtype (or bird flu), which typically circulates within wild bird populations. First identified in 1997, recent outbreaks of the now dominant strain, which is spread by migrating birds, have resulted in tens of thousands of avian deaths in the UK alone. Asymptomatic wild aquatic birds can also act as vectors for the disease, resulting in outbreaks in domestic poultry.
Asymptomatic wild aquatic birds can also act as vectors for the disease, resulting in outbreaks in domestic poultry.
Whilst primarily an animal disease, H5N1 can infect humans through close or prolonged contact with infected birds or their bodily fluids, such as saliva and faeces. The severity of infection varies, ranging from asymptomatic to severe upper respiratory illnesses like pneumonia, which can lead to death. Since 1997, the World Health Organisation (WHO) has recorded almost 1000 cases globally, with a concerning fatality rate of approximately 50%.
A troubling increase in mammalian infections
Worryingly, spillovers of the virus from birds to other animals, especially mammals, have been detected recently, with a concerning spread across dairy cattle farms in the USA since late January 2024. A preprint from November 2024 suggests that this circulating strain has a greater risk of causing a pandemic than historical strains due to its increased ability to bind to certain human cells.
In America, the Centre for Disease Control (CDC) is closely monitoring the situation, having tested over 600 individuals and coordinating with the WHO. Simultaneously, the US Department of Agriculture (USDA), US Food and Drug Administration (FDA), and CDC have implemented milk safety surveillance measures to prevent further spread from cattle. Despite this monitoring, the US infection count has now reached 67, with its first human death recently reported in Louisiana. A second human case of avian flu was detected in England, although the strain was different from that currently circulating in the US.
…the US infection count has now reached 67, with its first human death recently reported in Louisiana.
The risk to the public is currently considered low by the CDC, as, crucially, there is no evidence to date of human-to-human transmission. However, individuals who handle birds, whether for work, backyard farming, or recreational reasons, are at risk of infection. The WHO recommends avoiding contact with sick or dead wild birds and poultry, wearing personal protective equipment (PPE), and reporting any sick birds that may be potential sources.
Early detection is critical for minimising contact and monitoring how the virus is changing over time, as each human infection provides the virus with an opportunity to adapt for better transmission between humans.
Could H5N1 mutate for human transmission?
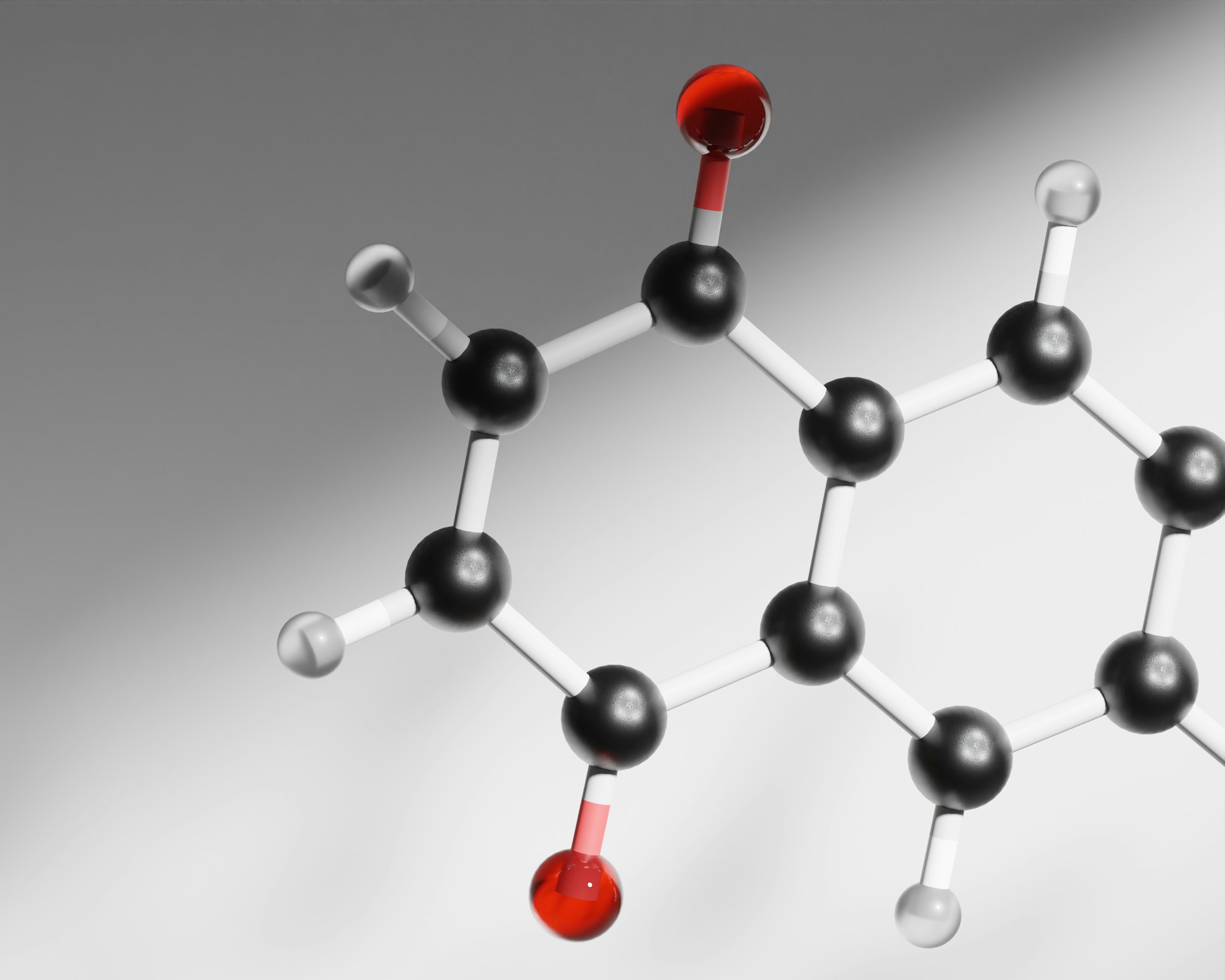
The “H” and “N” in H5N1 stand for the proteins hemagglutinin and neuraminidase. Hemagglutinin is needed for the virus to attach to host cells, while neuraminidase helps release new virus particles from infected cells. Last week scientists showed that a single mutation in the hemagglutinin protein could enable H5N1 to shift its binding preference from avian to human cell receptors The discovery of this mutation was particularly alarming as previous research suggested that at least two mutations were necessary for this change to take place.
So far, there is no evidence that this same specific mutation has emerged in animal populations. However, sequencing data from an infected Canadian teen revealed that some viruses had mutated in a similar way. While the change was not the same as described above and did not lead to increased human receptor binding, this research demonstrated that the site is able to mutate.
…we may not have yet identified all the possible barriers to human infection and transmission.
Despite these studies, we may not have yet identified all the possible barriers to human infection and transmission. During spillover infections, H5N1 viruses can adapt to human infection in unexpected ways through mutation or reassortment, where different influenza viruses exchange genetic material when they infect the same host, sometimes creating entirely new viral strains with altered virulence or transmissibility. In addition, some scientists argue that there is also a risk posed by viral research, stating that lab-based mutation experiments pose a greater risk of accidental release than the natural evolution of the virus itself.
What countermeasures are in place?
Currently, the main medical countermeasure against H5N1 is the use of the influenza antiviral drug Oseltamivir to treat individuals who were in contact with infected birds.
At the moment, no human vaccination against bird flu is recommended, and seasonal flu vaccines are unlikely to provide protection to H5N1 according to the European Medicines Agency (EMA). There are three vaccines designed to protect birds are authorised for use in the EU and are effective for reducing the spread alongside animal culling.
Several human vaccines for previous strains of H5H1 have also been developed and are retained in stockpiles in America that are likely to provide some protection against severe infection. The UK Government also agreed to purchase over 5 million doses of a human H5 influenza vaccine from CSL Seqirus in December 2024 to ensure that vaccines are immediately available if needed.
…four pandemic preparedness vaccines are authorised for fast-track approval.
Additionally, candidate vaccine viruses have been developed by the CDC and shared with manufacturers in the US. In Europe, four pandemic preparedness vaccines are authorised for fast-track approval due to previous safety and efficacy tests, allowing rollout in only 70 days as opposed to the usual 210 or more days. Currently, mRNA candidate vaccines that use the same technology as some COVID-19 vaccines are in the early stages of testing.
What happens next?
The potential for H5N1 to mutate and acquire human-to-human transmissibility remains a significant concern yet is an inherently unpredictable possibility. The Trump administration’s decisions to withdraw funding from the WHO and to restrict CDC communication of bird flu updates further complicate the picture. As aptly noted by Nobel laureate Norman Borlaug, “The greatest ally of the pathogen is our short memory…,” a sentiment that feels particularly relevant as we move on from the COVID-19 pandemic.
The UK’s recent expansion of the Avian Influenza Prevention Zone, which mandates enhanced biosecurity measures, is a positive step, but sustained and global efforts will be crucial to mitigate the risks posed by H5N1 and other emerging infectious diseases.