Could a vaccine answer our cancer questions? Photo credit: National Cancer Institute via Unsplash
LungVax is an exciting new initiative driven by the University of Oxford, University College London, and the Francis Crick Institute, funded by Cancer Research UK and the Cancer Research Innovation in Science (CRIS) Cancer Foundation, that seeks to develop an unparalleled vaccine to treat non-small cell lung cancer (NSCLC).
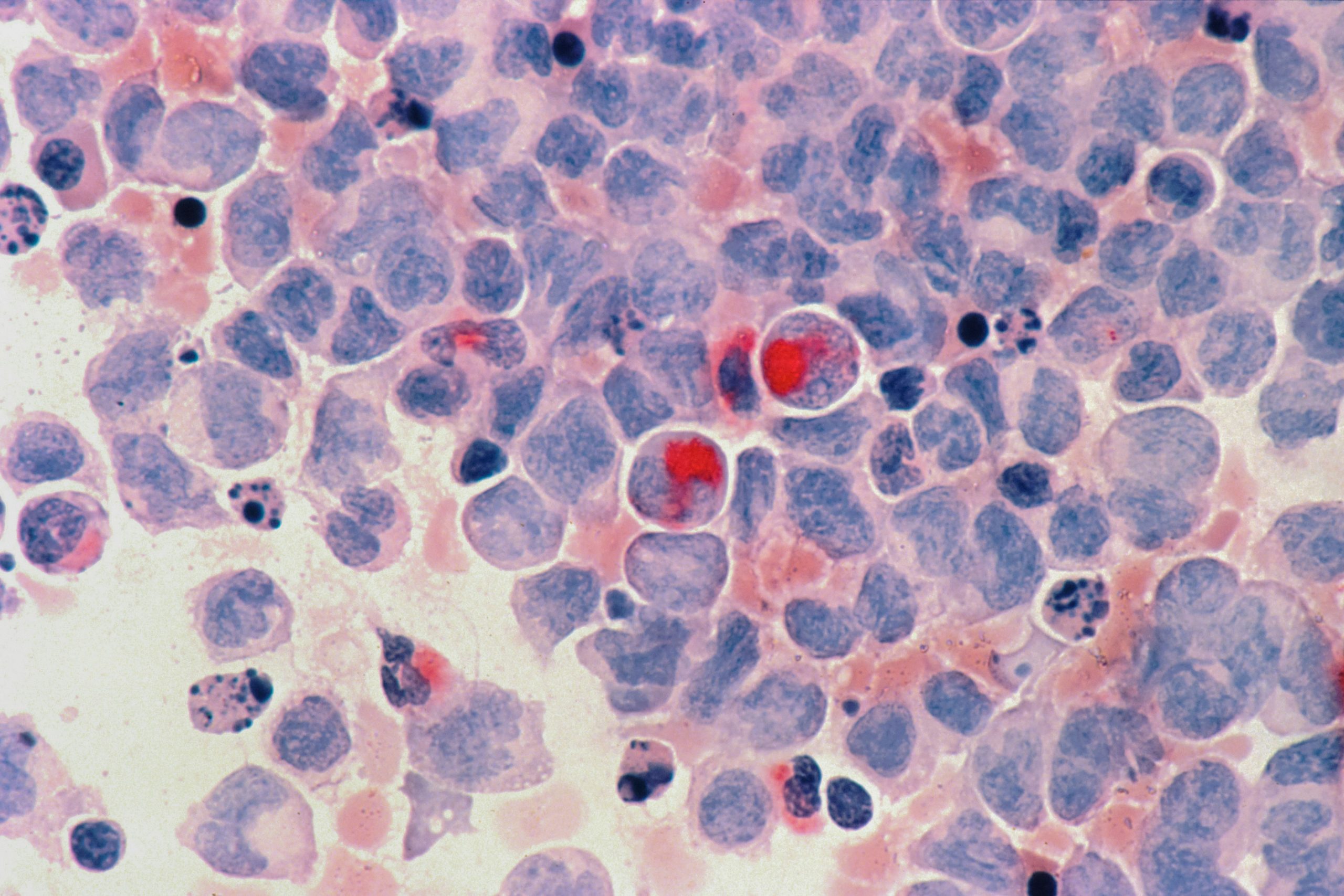
The term cancer refers to a multitude of diseases characterised by the uncontrolled division of abnormal, genetically mutated cells that form tumours. These tumours can then metastasise or spread to other parts of the body by entering the bloodstream and invading foreign tissue. There are a few main categories of cancer, classified by the type of tissue they originate in, including sarcoma, leukaemia, lymphoma, myeloma, and the most common: carcinoma. Carcinomas form in epithelial tissue, tissue that lines and covers surfaces in the body, sarcomas form in connective tissue, and leukaemias form in white blood cells. Cancer is malevolent, hijacking normal biological processes to support its uncontrolled growth at the expense of its host organism. It does this by employing covert strategies, undetected by its host organism, evading the immune system, resisting programmed cell death (apoptosis), inducing novel blood vessel formation (angiogenesis), and stimulating metabolic reprogramming to make our bodies its unwelcome home. The irony is that cell division, the process gone haywire in cancer, is also fundamental to life.
…diseases characterised by the uncontrolled division of abnormal, genetically mutated cells that form tumours.
When examining lung cancer specifically, approximately 80-85% of cases are NSCLCs, consisting of carcinomas. It is the third most common cancer in the UK, with 130 new cases daily. Smoking is one of the most preventable risk factors for lung cancer, yet it causes over seven out of every 10 cases. Despite its high preventability and ongoing education to reduce its incidence, the ubiquity of lung cancer definitively marks the urgent need for novel and effective treatment, as promised by LungVax.
Smoking is one of the most preventable risk factors for lung cancer, yet it causes over seven out of every 10 cases.
How does LungVax work?
The somatic cells comprising our body are identified by our immune system as being ‘self’ by the presence of self-antigens, ensuring that they do not stimulate an immune response. Antigens are found on the cell surface of invading microbes like bacteria and viruses and diseased cells like cancer. They are identified by macrophages and lymphocytes that mount an immune response against them through the production of antibodies. However, cancer cells do not only present self-antigens but also neoantigens—abnormal cell surface proteins arising from genetic mutations. These neoantigens are recognised as foreign by the immune system and offer a target for immunotherapy—cancer therapy, which harnesses or enhances the immune system to fight and destroy cancerous cells.
cancer cells do not only present self-antigens but also neoantigens…
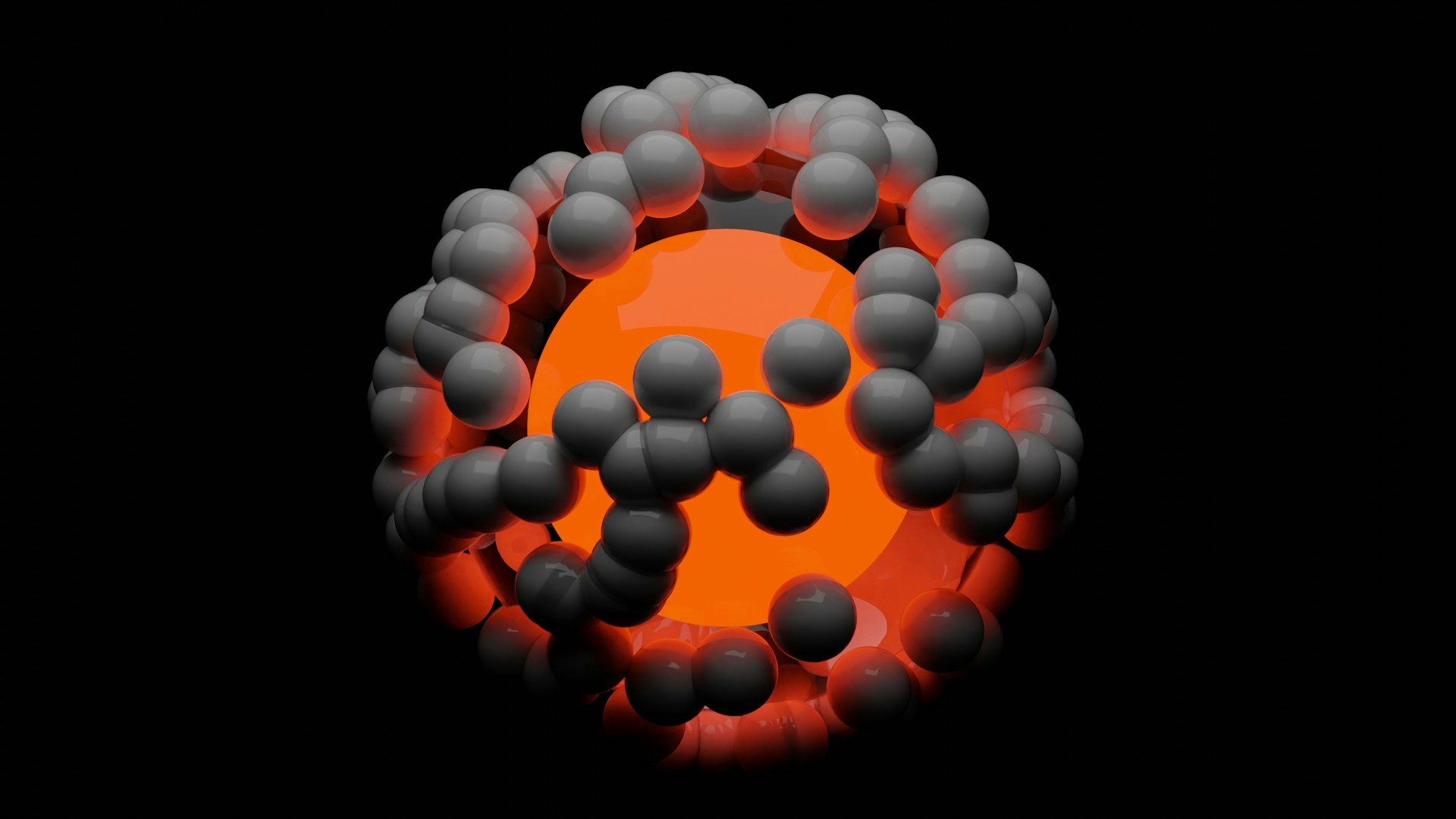
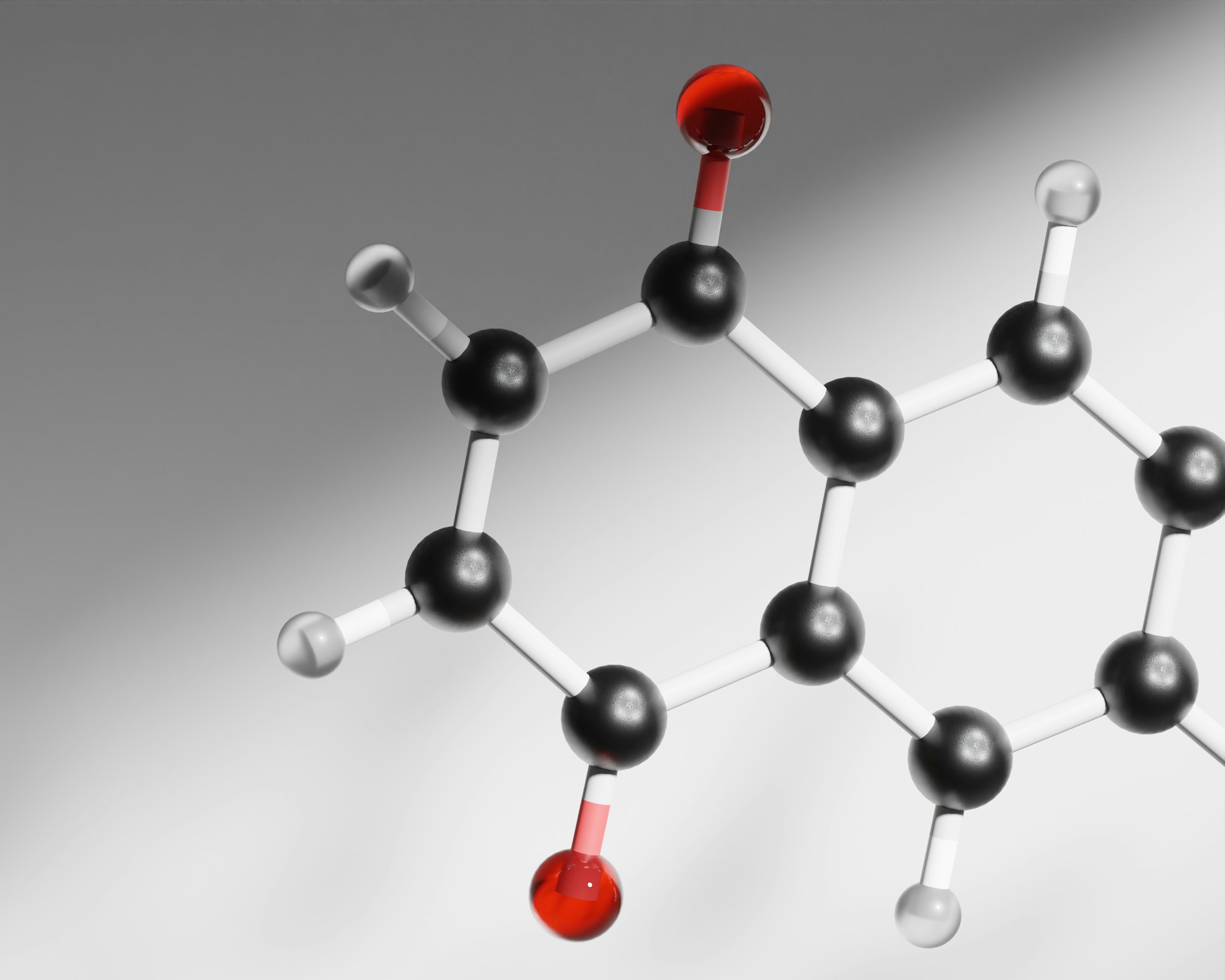
Neoantigens serve as the foundation for LungVax’s mechanism of action. LungVax works via an mRNA mechanism similar to Oxford–AstraZeneca COVID-19 vaccine technology. In these vaccines, mRNA encoding a protein of interest is delivered to cells via viral vectors. The mRNA is then translated into the protein of interest by the cell’s ribosomes. These proteins are often antigens or spike proteins found on viruses, bacteria, and abnormal ‘self’ cells like cancer. In the Oxford-AstraZeneca vaccine, the mRNA encoded for a spike protein found on the surface of the COVID-19 virus. However, in LungVax, the mRNA strand encodes the instructions for making the neoantigens seen on NSCLC cells.
As we encourage the body to produce these molecules, we train our immune system to recognise and destroy cells that display NSCLC neoantigens. Consequently, by administering this vaccine to individuals with early-stage lung cancer, we can stimulate the elimination of NSCLC cells, increase the efficacy of other anti-cancer treatments, and even prevent its formation in those with a high risk of developing it.
What makes LungVax different?
The current predominant form of lung cancer immunotherapy lies in drugs such as pembrolizumab and atezolizumab—known by their more pronounceable brand names, Keytruda and Tecentriq. However, immunotherapy drugs only treat patients with existing cancer, are administered after a cancer diagnosis, and often come with side effects like nausea and hair loss. They also have broad action, targeting multiple pathways in the immune response, which can complicate treatment plans and require diligent patient monitoring and management of side effects. Although still in development, LungVax would most likely have side effects seen with other vaccinations, namely, flu-like symptoms, inflammation, and skin irritation at the site of injection, but will not generate long-term consequences like autoimmunity seen with some immunotherapy drugs. Additionally, the specificity of LungVax grants it a range of advantages, including a targeted and efficacious immune response through precise neoantigen recognition, potential for combination therapy, reduced risk of autoimmunity, and long-term immune memory against NSCLC cells.
…the specificity of LungVax grants it a range of advantages.
However, what makes LungVax a potential breakthrough is its preventative capacity. Although refraining from smoking remains the most effective way to prevent lung cancer, this vaccine could provide protection for smokers and individuals with a heightened genetic risk. This would allow precision medicine approaches tailored to a person’s unique genetic makeup, further enhancing vaccine efficiency. It would protect them against developing NSCLC in the future by priming the immune system for any potential tumour formation, something immunotherapy drugs are unable to achieve. Lola Manterola, President of the CRIS Cancer Foundation, stated that LungVax is a pioneering vaccine that uses ‘technology and knowledge of the immune system […] to take the first steps towards preventing cancer [as opposed to only treating those already with lung cancer].’ This is an exciting venture that, while likely to take a few years to test and develop fully, displays massive clinical potential and could reshape the landscape of cancer treatment for other types of cancer as well.
…this vaccine could provide protection for smokers and individuals with a heightened genetic risk.
As one of the first groundbreaking genomic technologies being tested for preventing and treating cancer, LungVax represents the incredible culmination of the progressive strides genomic medicine and oncology have made in the past few decades, opening the door for other ingenious innovations. This therapy may still be in its infancy, requiring at least another few years to completely develop and implement; however, when successful, we can hope to see it transform thousands of lives worldwide, spurring us closer to a future where we can finally breathe—knowing that lung cancer is on the endangered list.