Introducing animal organs into humans is often considered an ethical slippery slope. But, could this prove to be a useful technique at a time where organ donor shortages are rampant? Image credit: Ben Mater via Unsplash
Organ xenotransplantation, or the transplantation of organs between species, is a field of research that has encountered substantial challenges in feasibility, safety, and ethics. Despite these hurdles, it persists as a promising solution to address human donor organ shortages. In a significant stride towards making this a reality, researchers in the USA have now demonstrated that a monkey was able to survive over two years with a kidney from a genetically modified pig donor.
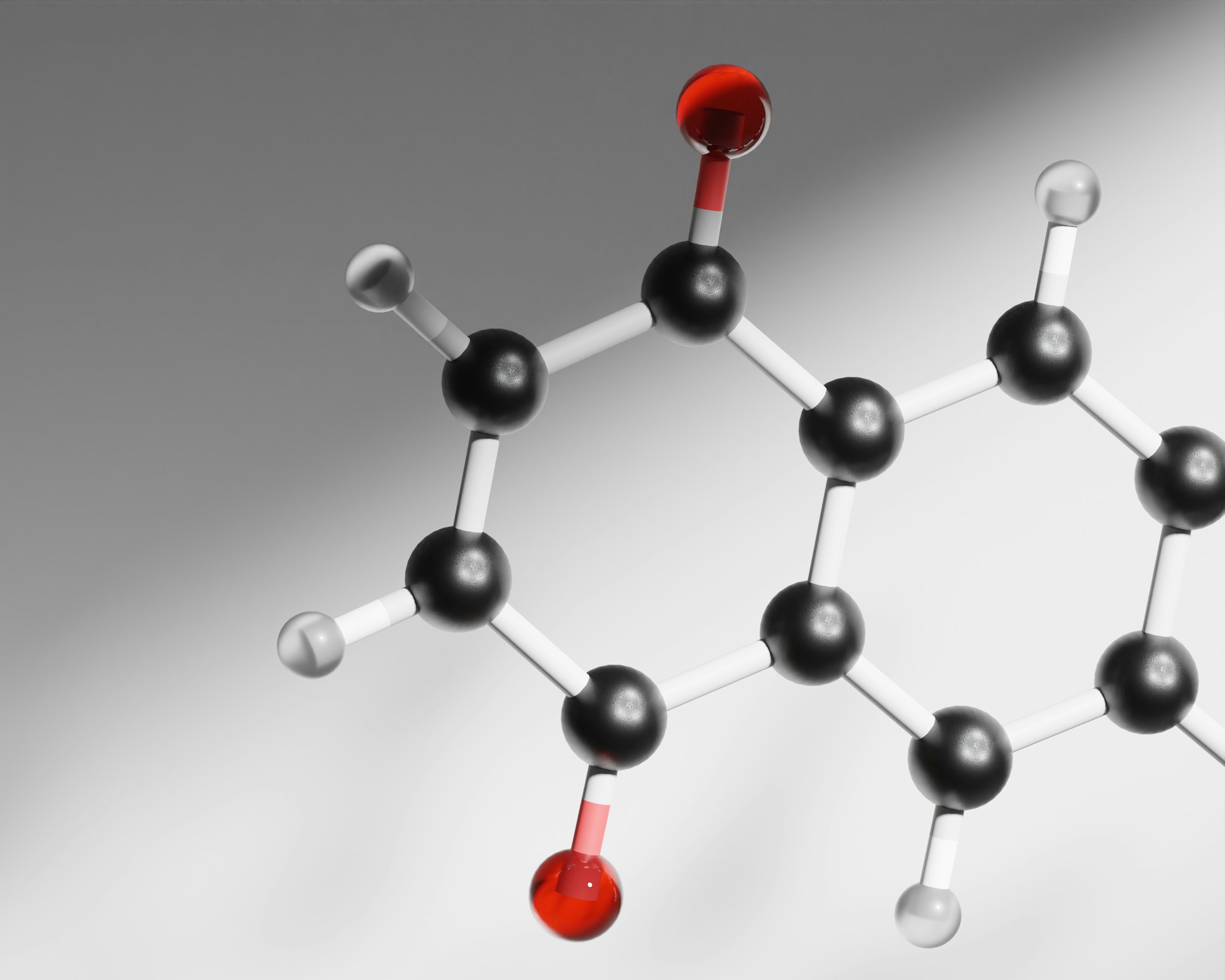
In a collaborative effort between scientists at the gene editing firm eGenesis and Harvard Medical School, researchers successfully designed porcine kidney donors harbouring over 60 gene edits. Carefully constructed to make the donor kidney more compatible with the human immune system, these strategic edits included the deletion of three pig glycan antigen genes, mitigating rejection risk. Additionally, they introduced and overexpressed seven human transgenes related to processes such as immunity and blood coagulation, fostering healthy kidney function and minimising damage. Porcine retrovirus sequences (which comprised 59 of the edits) in the pig genome were also deleted to eliminate the risk of these viruses transmitting into other species.
The researchers tested four distinct donor kidney types with varying combinations of modifications using both in vitro (lab-based) and in vivo (in living organisms) methods. The donor kidneys were first incubated in serum collected from both monkeys and humans to determine how they would react to the foreign kidney in vitro. Next, they transplanted the kidneys into 21 non-human primate models and monitored them for healthy kidney functioning and signs of damage.
The results were clear—the donor kidneys with both glycan antigen knockouts and the human transgenes exhibited superior survival and kidney health to those with only one or the other. Remarkably, one monkey survived for 758 days with the donor kidney, and another four monkeys surviving for more than a year. (At date of publication, two of these were still alive). These survival times are a significant advancement from those seen in other studies, which have previously only achieved a maximum post-transplant survival of 316 days. In vitro testing also confirmed that the kidneys with human transgenes experienced better blood clotting and reduced inflammation and immune activation. Altogether, these results suggest that the addition of human transgenes to genetically modified porcine donors is a key step to promoting organ survival after transplantation.
This research comes at a critical time amidst donor organ shortages and growing demand globally, linked to ageing populations and growing incidence of non-communicable diseases.
This research comes at a critical time amidst donor organ shortages and growing demand globally, linked to ageing populations and growing incidence of non-communicable diseases. In the UK, the NHS estimates that there are over 7000 patients currently on the organ transplant waiting list, and in the US, approximately 17 people die each day waiting. Two previous pig-human heart xenotransplantation attempts have been broadly unsuccessful, with both patients unfortunately surviving less than two months post-operation. However, their donor hearts held only ten gene edits and likely contained retrovirus sequences, with the activation of one of these viruses tentatively attributed to the death of one patient. Therefore, this research holds promise as it demonstrates that a donor kidney with both a greater number of gene edits and the deletion of retroviruses could achieve better clinical outcomes. Moreover, the researchers note that in the future, genetically modified organs could be personalised to the recipient’s unique biology, minimising the need for extensive immunosuppressive regimens and their associated risks.
In the UK, the NHS estimates that there are over 7000 patients currently on the organ transplant waiting list, and in the US, approximately 17 people die each day waiting.
Despite these promising outcomes, the path to kidney xenotransplantation in human clinical trials remains uncertain. Monkey survival post-transplant was highly variable within the trial, with some of those receiving the ‘optimum’ modified kidney still surviving for less than a month. Meanwhile, the small study size and the non-random nature of the trial (monkeys were pre-selected based on having lower antibody reactivity to the donor kidneys) raise broader questions about the applicability of this research. Despite the researchers’ efforts to include in vitro human testing, there is no guarantee that these results will translate to success in human clinical trials. Ethical concerns surrounding animal welfare, genetic engineering, and religious objections also further complicate the trajectory of xenotransplantation.
Of course, there are also many other ways of solving the donor organ shortage. Scientists have already managed to successfully grow organ-like structures (known as organoids) entirely from human stem cells, and 3D printing of organs has also been suggested as a tool. Being entirely lab-based, these methods offer us a more ethical manner of supplying donor organs in future. Researchers are even looking into the prospect of repairing or regenerating damaged organs entirely using bioengineering, which could put an end to the long waiting lists for good. Whilst we wait for these technologies to be developed, policies such as recent steps in many countries to make organ donation an ‘opt-out’ process can also play a key role in maintaining the availability and efficient allocation of donor organs.
At present, organ xenotransplantation from humans to pigs is a highly experimental and controversial concept. However, this research remains an exciting step in the future of xenotransplantation, and one to watch out for should this technology reach human clinical trials.