MediaJet, CC BY-SA 3.0, via Wikimedia Commons
A Dutch and Scottish study recently reported that how we are born could alter the way in which our immune system responds to vaccines. They found that babies born vaginally had more protective antibodies after childhood vaccines, compared to babies delivered via caesarean section.
The researchers suggested that this difference is due to the types of good bacteria that colonise our bodies at birth.
It is important that we be exposed to good bacteria early in life, as this makes up our microbiome (the community of microorganisms that live within our bodies). The microbiome trains our immune system in early life so that we are protected and ready for future infections.
At birth we are immediately exposed to a world full of microbes—some are good, and some can be bad for us.
If born through the birth canal, the first microorganisms you meet are the ones that live in the vagina, whereas delivery via C-section means initial exposure to microbes will be to those on the skin, or in the hospital or at home.
It is known that gut bacteria (which comprise our gut microbiome) release chemicals called short chain fatty acids that signal to the immune system to engage its fighters. Without this signalling from our gut microbiome, we would see impaired B cell development. These cells are essential for the production of antibodies and therefore our response to vaccinations.
Since the first vaccine was designed in 1796 (Dr Edward Jenner’s smallpox vaccine), we have been able to manipulate the immune system to protect our bodies from the risk of infection by a variety of dangerous microorganisms.
Vaccination involves injecting a killed or weakened form of a harmful microbe into the body to elicit a response from our immune system with the aim of stimulating a specific-antibody response to counter the infecting microbe. Vaccinations mean that if we are exposed to the harmful microorganism again, in its natural form, we will already have some existing immunity against it, preventing infection or attenuating an infection’s consequences.
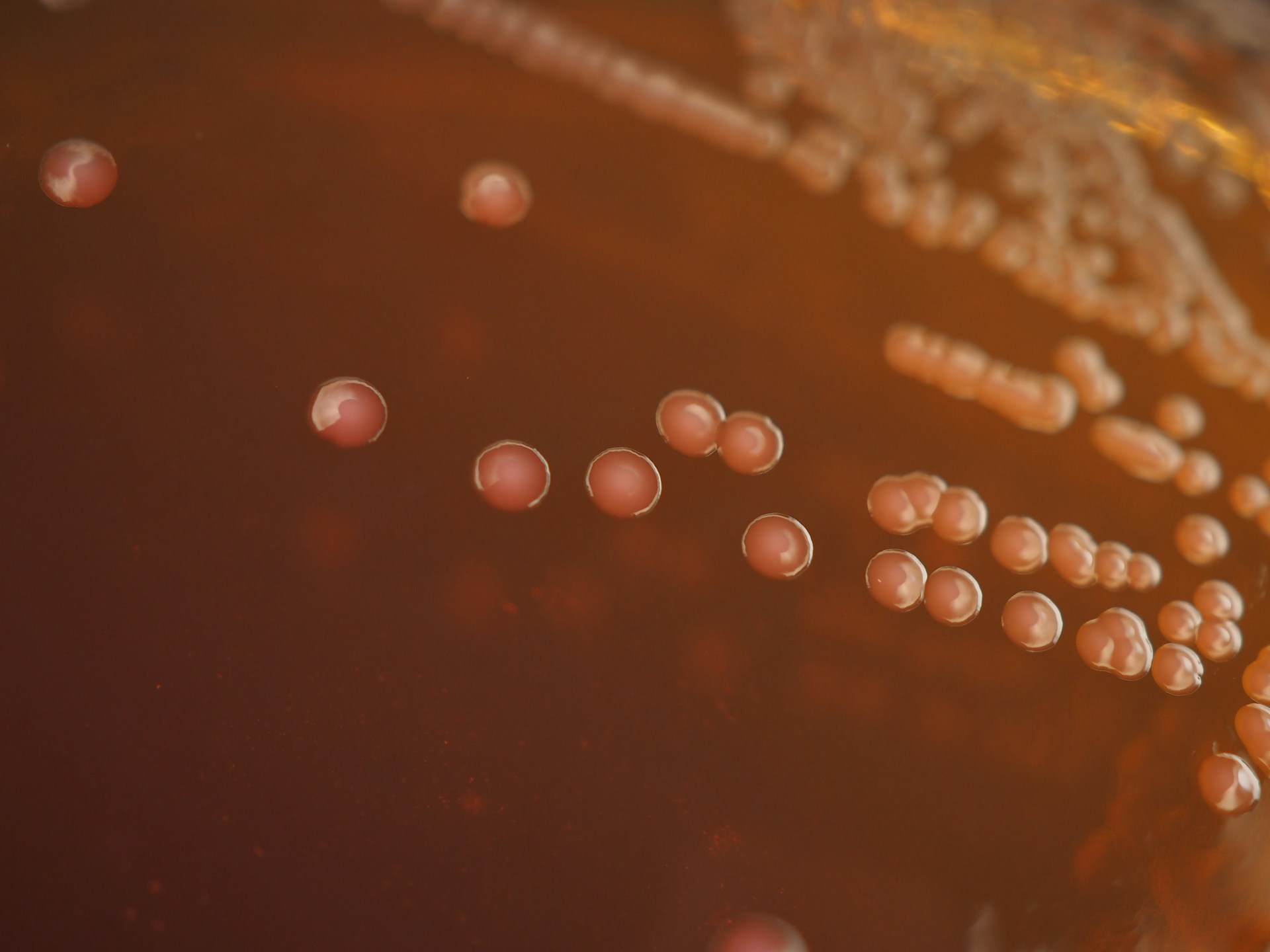
Researchers at the University of Edinburgh and Spaarne Hospital and Utrecht University Medical Centre in the Netherlands were interested to explore whether the mode-of-delivery, and thus types of bacteria babies are initially exposed to, influences responses to vaccines. They tracked the gut microbiome of 120 babies from their very first thick, green poo (the meconium) until they were a year old.
Their results, published in the journal Nature Communications, showed higher levels of Bifidobacterium and E. coli species (only a few strains of E. coli are harmful) in children born vaginally than those who were delivered via C-section. Vaginally delivered children showed a 1.7-fold higher antibody response to meningococcal vaccination and a higher response to pneumococcal vaccination, compared to C-section delivered infants.
In light of these two observations, the researchers suggest that the bacteria species found in higher levels in vaginally delivered children are beneficial and lead to this increased level of antibody production in response to both vaccines.
All babies in this study were healthy and had reached full term so the findings are not affected by other disease or premature birth.
However, the findings simply show a correlation between factors rather than causality. Further research is needed before it is safe and appropriate to draw firm conclusions. Additional factors that could alter our microbiome need to be investigated alongside mode-of-delivery, such as antibiotics treatment in infancy and exposure to air pollution.
While all children, whether delivered vaginally or by C-section, produced antibodies in response to vaccination, C-section babies had lower levels of antibody production, indicating less protection against infection.
So the question arises, what can be done to help protect C-section babies?
Although the researchers of this study suggest that discouraging the increasing application of C-section may be important to preserve the microbiome-immune axis in infants, C-sections cannot be entirely avoided as they are often medically necessary to protect the health of the mother or baby.
Therefore, methods to regulate the gut microbiome following C-section are vital for robust antibody responses to vaccines and to ensure that fully vaccinated infants are not left unprotected against severe infections.
“Vaginal seeding” is one method that has been suggested, whereby C-section babies are smeared with vaginal fluids from their mother in order to replace the microbes that were not encountered during delivery. However this can be complicated, and it is important to make sure that it is not dangerous.
Trials that have used faecal matter, transplanted from mother to baby, to introduce microbes to C-section babies have screened the faecal matter for dangerous infections. But this is not practical to do for every C-section baby and thus is not scalable.
To bypass the risk of introducing dangerous bacteria to the infant, giving the baby a cocktail of beneficial bacteria (i.e., a probiotic) has been investigated. Alternatively, C-section babies could be given an extra dose of any given vaccine to elicit a stronger immune response that would match that of vaginally delivered babies.
The findings of this paper are important in beginning to understand the factors that contribute to vaccine responses in infants and the role of the microbiome.
As vaccination in early childhood is estimated to save millions of lives each year, it is paramount that vaccination programmes are as robust as possible and take into consideration inter-individual variations in antibody responses to vaccines administered during infancy.