A new ultrasound-activated nanotechnology offers a promising way to selectively weaken liver cancer cells by exploiting an unusual form of cell death. Photo credits: Shubham Dhage via Unsplash
Researchers have developed a new nanotechnology that has demonstrated encouraging results in slowing the progression of hepatocellular carcinoma.
Hepatocellular carcinoma…is a major source of cancer-related mortality.
With people living longer than ever before, cancer is an ever-growing issue. It is a disease like no other, where the body’s cells go haywire and become uncontrollable, resulting in devastating effects. It takes many forms, but some are more difficult to deal with. Liver cancer is one such condition, with a survival rate of only 8% after 10 years. Hepatocellular carcinoma is the most common type, responsible for 90% of cases. Deep inside the body, quickly becoming resistant to our current arsenal of drugs, and usually only noticed in its later stages, this disease is a major source of cancer-related mortality. To tackle it, researchers from Guangxi and Beijing have developed a nanoparticle that aims to kill cancer cells using ultrasound.
The technology is based off a recently discovered method of cell death—ferroptosis. As the name might suggest, it depends on the behaviour of iron inside cells, and its interaction with how cells deal with oxygen.
Oxygen’s toll
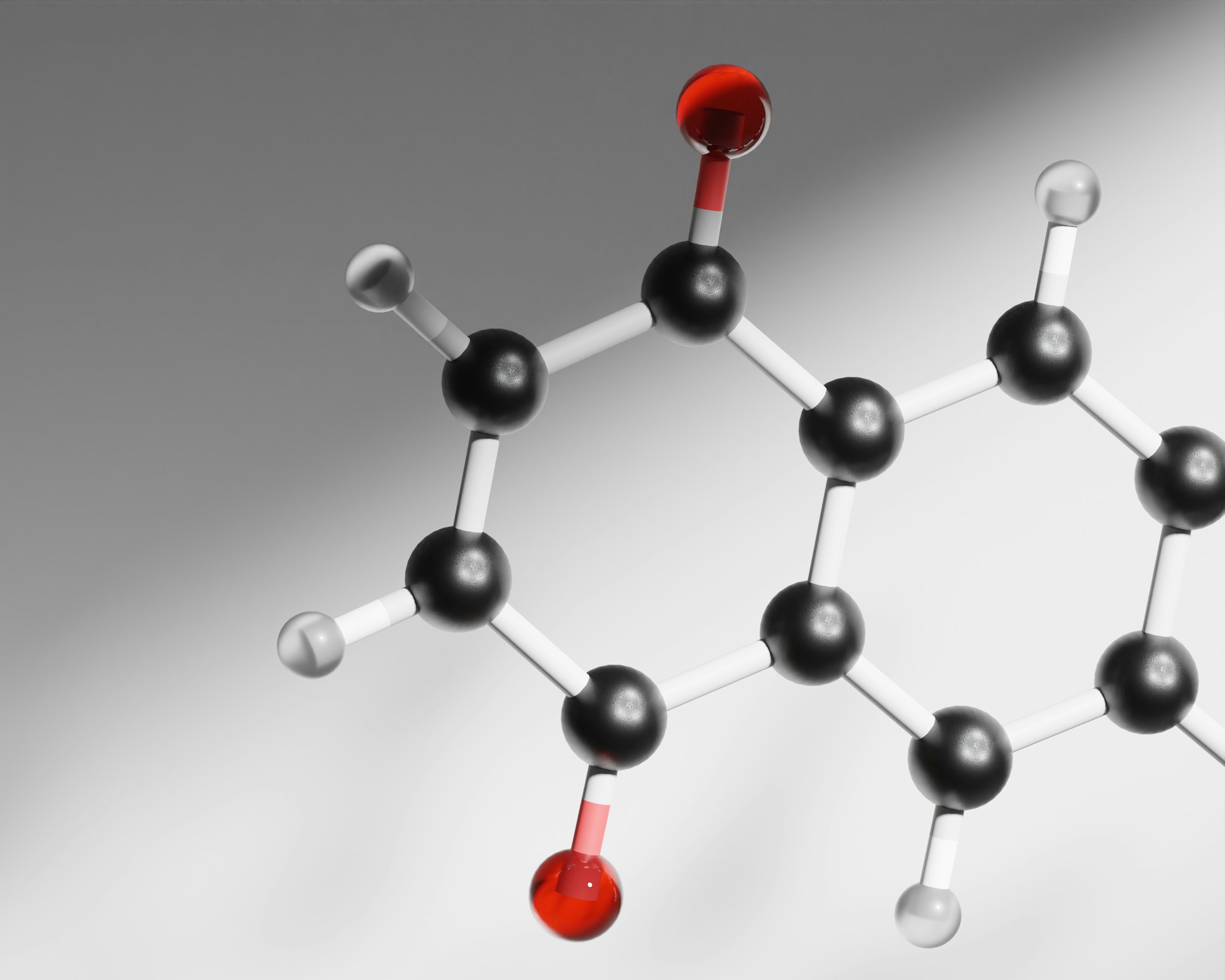
Oxygen is an incredibly dangerous element. If used carelessly (which cells very often do), it can generate a variety of unpredictable, reactive, and unstable compounds known as reactive oxygen species (ROS). Moreover, oxygen gas itself also reacts with a variety of different compounds. The inner lining of the cell membrane contains lipids that are exposed to the volatile environment inside cells. These lipids can be oxidised in a controlled manner using enzymes to control their host cells, but they can also be oxidised spontaneously by oxygen or ROS. This leaves a peroxide group on the lipid. Peroxidation is quite unhealthy for cells, as the peroxide group gives lipids new properties that interfere with the cell membrane, making it thinner and less flexible.
Iron can then convert these peroxides into peroxyl radicals. With a name like that, it is unsurprising that these are terrible for cells, as they actively make more peroxides and generally wreak havoc on the membrane. While a single peroxide won’t kill a cell, added up, these molecules can compromise the cell membrane, which is the critical step required to kill a cell.
Obviously, healthy cells don’t just sit around and wait for their oxygen addiction to kill them; they have methods to slow and undo this peroxidation. Cells use the enzyme GPX4 to convert peroxides into less dangerous alcohols. It does this using glutathione (GSH), which gets oxidised and can then be processed safely. Similarly, GSH also soaks up ROS found in the cytoplasm, and this is what makes it an antioxidant. Cells also process Vitamin K into another powerful antioxidant—hydroquinone. This compound is made by the enzyme VKORC1L1, soaking up ROS to inhibit lipid peroxidation. Cancer cells exploit these two systems to evade ferroptosis and stay safe. It is these systems that the invention targets.
How to build your nanoparticle
The particle is made from a simple three components. The general structure is provided by DSPE-PEG2000, a commonly-used lipid compound that gathers to form tiny spheres when in water. Inside these spheres, the researchers used the inhibitor warfarin, which is capable of shutting down the activity of the VKORC1L1 enzyme. Warfarin was previously known to inhibit tumour growth in mice, but challenges in ensuring it only targets cancer cells without causing side effects meant that this therapeutic needed improvement. This is where the most innovative part comes in; the researchers then invented their own biodegradable sonodynamic polymer (BSD) that gets woven into this sphere when it forms. This BSD polymer is special, as it contains a donor-π-acceptor-π motif, a structure that is very good at moving electrons and generating ROS from this activity, when exposed to ultrasound. The polymer was also designed to be easily degraded in the presence of ROS, which in turn disassembles the entire particle.
In short, once these particles enter cancer cells, all that professionals need to do is focus ultrasound onto the tumour—technology that we have been improving upon for decades. This generates huge quantities of ROS that disassemble the particle, damage the cell, and use up huge amounts of GSH, weakening this defence system. Additionally, the researchers found that this also significantly inhibited GPX4 expression, further increasing peroxidation. Meanwhile, as the particle falls apart, the warfarin inside is released, shutting down hydroquinone production by inhibiting VKORC1L1. Combined, these effects increase peroxidation sufficiently to trigger ferroptosis, killing the cancer cell, and only the cancer cell.
Combined, these effects increase peroxidation sufficiently to trigger ferroptosis, killing the cancer cell, and only the cancer cell.

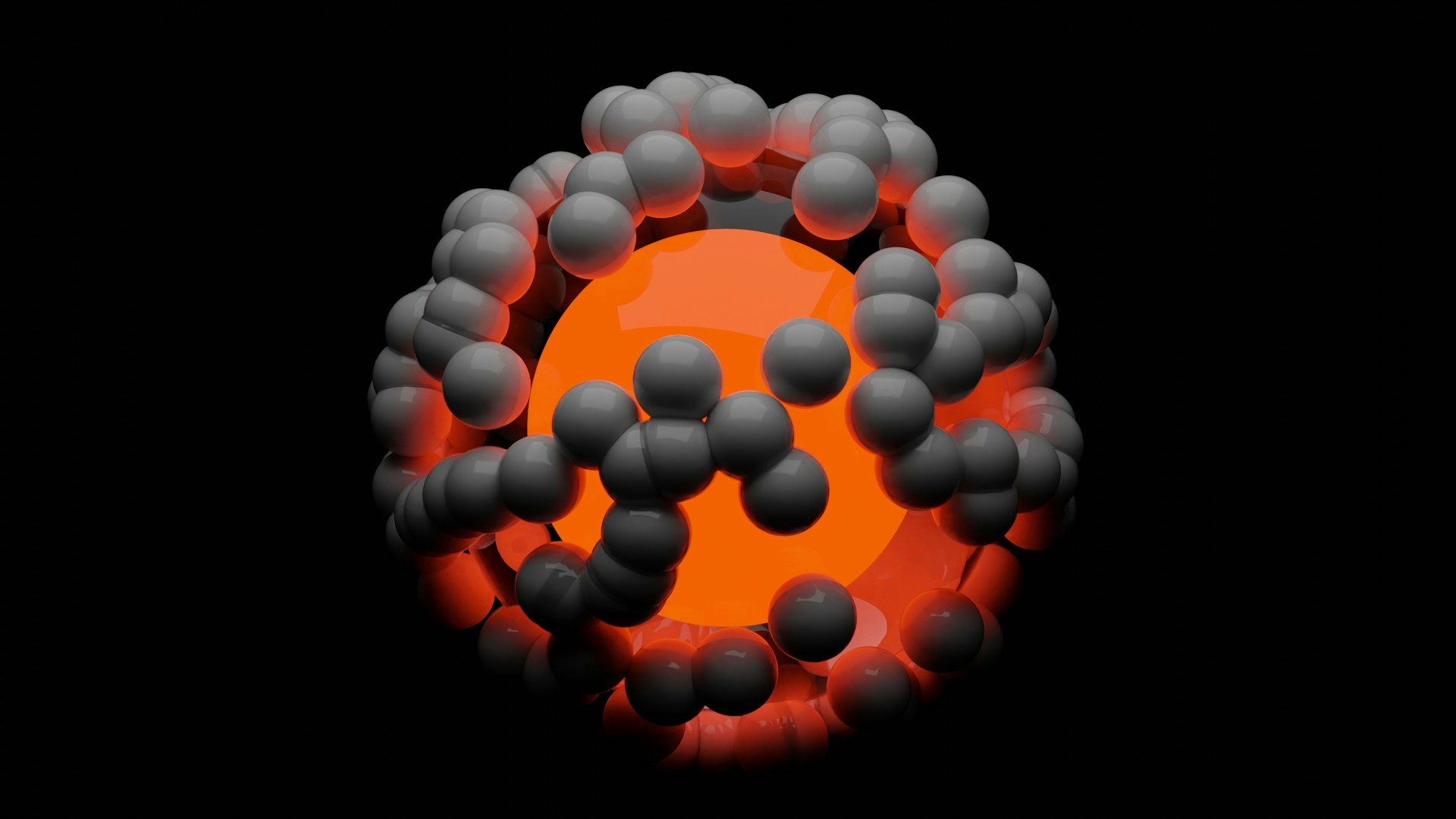
Figure 1: The graphical abstract of how the invention works.
In their paper, the researchers also tested how their particle behaved in mice. It behaved largely as expected, accumulating in tumour cells, not remaining in the blood for too long after injection, and not causing any damage to other parts of the body (which is rather important for a therapeutic). Excitingly, mice treated with the nanoparticle and ultrasound fared significantly better than untreated mice, showing massively reduced tumour sizes and tumour weights without any changes in body weight that would indicate side effects.
The treatment produced a tumour inhibition rate of 92% after 12 days, significantly slowing tumour growth
The study also revealed that ferroptosis caused by the nanoparticle-ultrasound combination activated the immune system. The number of mature dendritic cells in lymphatic tissues and the number of T-cells in the tumour both significantly increased, indicating an enhanced immune response against the tumour. The treatment produced a tumour inhibition rate of 92% after 12 days, significantly slowing tumour growth.
The trials ahead
Unfortunately, use of this strategy in hospitals is still a long way off. While their studies showed promising signs, the researchers themselves stated that they did not ‘directly demonstrate therapeutic efficacy’. It is still unproven whether this treatment would actually prolong the lives of mice with tumours, let alone humans. It is also worth considering that, as liver cancer tends to only be noticed and diagnosed in its later stages, the treatment may not prove very helpful in this context. Nevertheless, if promising results persist from future studies and clinical trials, we could weaponise ferroptosis against other cancers that are potentially vulnerable to this strategy. Then, this therapy may join the ever-growing toolkit of methods to beat cancer.